New standards for brain organoids aim to boost drug discovery
Posted: 22 July 2025 | Drug Target Review | No comments yet
A new international framework introduces rigorous validity standards for the use of brain organoids and iPSC-derived models in studying neuropsychiatric disorders. These guidelines aim to accelerate drug discovery and bring precision treatments closer to reality.
Neuropsychiatric disorders are among some of the most complex medical conditions – affecting more than 3 billion people worldwide. Despite decades of research in genetics, scientists have struggled to translate laboratory discoveries into effective, patient-tailored treatments. This “translation gap” has left clinicians with few tools to deliver the promise of precision medicine.
Now, in a comprehensive peer-reviewed perspective published in Genomic Press, an international team of neuroscientists led by Dr Nael Nadif Kasri at Radboud University Medical Center has proposed a new approach to help close that gap. Their work focuses on establishing rigorous standards for using induced pluripotent stem cell (iPSC) models to study brain disorders.
“Human iPSC-derived two-dimensional neurons and glia, and three-dimensional organoids recapitulate key aspects of brain development and cellular functions,” the authors write, emphasising how these models reflect the exact genetic makeup of patients with neuropsychiatric disorders.
Three pillars of validity
At the centre of the framework are three types of model validity – construct, face and predictive – adapted from preclinical animal research and now tailored for use in human iPSC systems.
- Construct validity ensures that the model includes the correct disease-causing genes and relevant brain cell types. For rare, monogenic disorders like Rett syndrome, this may be straightforward. However, for complex, polygenic conditions like schizophrenia, which involve thousands of genetic variants, achieving construct validity becomes much harder.
- Face validity assesses whether cellular models resemble the disorder they’re intended to simulate. In neuropsychiatry, where diagnoses are based on symptoms like delusions, mood swings or cognitive impairment, researchers must instead rely on molecular or electrophysiological signatures. One promising method involves microelectrode arrays that capture electrical activity mirroring abnormal electroencephalography (EEG) patterns found in patients.
- Predictive validity gauges whether the model can accurately forecast patient treatment responses. In one study, iPSC-derived neurons from patients with bipolar disorder responded differently to lithium, matching clinical outcomes. This suggests that drug responses could be evaluated in the lab on a patient-specific basis.


Interdependency of construct, face, and predictive validity. Construct, face, and predictive validity are highly interdependent. Depending on the available information, a model system can be built starting at any of the three validities. Credit: Nael Nadif Kasri
Navigating technical hurdles
Despite their promise, iPSC models present many technical challenges. For example, reprogramming cells can introduce unintended genetic changes. The authors caution that “regular genomic integrity assessments” are essential to prevent misleading results.
Another issue is cellular diversity. Brain disorders often affect multiple regions and cell types, making it essential to select the appropriate cell populations for study. However, most current models reflect early foetal brain development, while many psychiatric conditions appear during late adolescence or adulthood – a mismatch researchers must address.
Examples of validation in action
The article highlights powerful examples of how these validity standards can be applied in practice. One study on 22q11.2 deletion syndrome – a known genetic risk factor for schizophrenia – combined brain imaging with iPSC-derived dopaminergic neurons. The results showed altered dopamine metabolism, a well-established mechanism in the disorder.
The article highlights powerful examples of how these validity standards can be applied in practice.
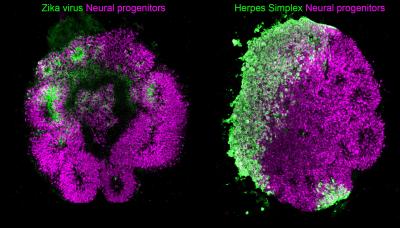
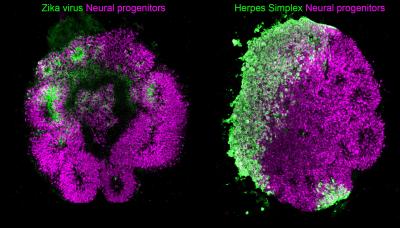
Similarly, brain organoids have shown oscillatory activity that mimics neonatal EEGs. In models of Rett syndrome, these organoids produced epileptiform activity, which could be weakened with therapeutic compounds – illustrating potential for drug discovery.
Future directions and big questions
The authors propose a flexible framework that allows researchers to begin with any validity pillar – depending on the available data. For example, if a treatment’s efficacy is already established, predictive validity may serve as an appropriate starting point.
They also raise important forward-looking questions:
- How can environmental risk factors be modelled alongside genetics?
- Could composite validity scores guide model selection?
- Might artificial intelligence detect subtle disease-relevant patterns that escape human observation?
Personalised medicine is another exciting area of study. Because iPSCs are generated from individual patients, they can capture unique genetic combinations. This allows researchers to simulate and treat highly specific or rare disease variants.
Implications for drug development
Validated iPSC models could change psychiatric drug pipelines – which have stalled for decades. The ability to model patient-specific responses could allow researchers to identify new drug targets, reduce clinical trial failures and tailor treatments with better precision.
Validated iPSC models could change psychiatric drug pipelines – which have stalled for decades.
The authors suggest combining electrophysiology, molecular profiling and drug testing into integrated approaches. This multi-modal validation could lead to shared disease mechanisms – even across genetically diverse patient populations.
Collaboration is key
To implement this framework at scale, the research calls for collaboration across disciplines – especially with clinicians who can provide insight into patient phenotypes and treatment histories.
They also recommend the creation of international consortia and model repositories, complete with standard operating procedures and validation data. This would enable scientists worldwide to work from consistent and reliable platforms.
Toward a future of precision psychiatry
With the global burden of neuropsychiatric illness continuing to rise, the need for more accurate, reliable and translational disease models is more urgent than ever. This comprehensive validity framework helps ensure that iPSC-based discoveries don’t just stay in the lab but reach the patients who need them the most.
By bringing together scientific innovation with clinical relevance, researchers are taking a vital step toward precision psychiatry – where treatments are tailored not to broad diagnostic labels, but to individual biology.
Related topics
Assays, Biomarkers, Cell Cultures, Drug Discovery, Induced Pluripotent Stem Cells (iPSCs), Neurosciences, Organoids, Precision Medicine, Translational Science
Related conditions
Neuropsychiatric disorders
Related organisations
Radboud University Medical Center
Related people
Dr Nael Nadif Kasri (Radboud University Medical Center)








