Eosinophilic esophagitis may be due to missing SPINK7 protein
Posted: 11 June 2018 | Drug Target Review | No comments yet
NIH-funded study finds replacement therapy reversed effects in tissue experiments…
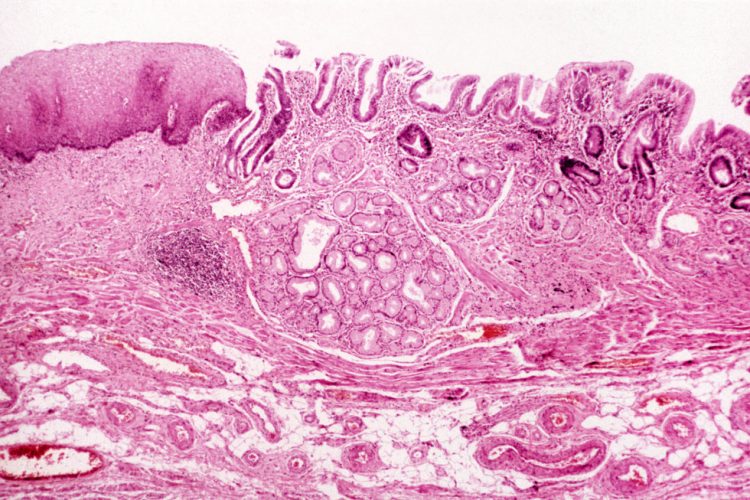
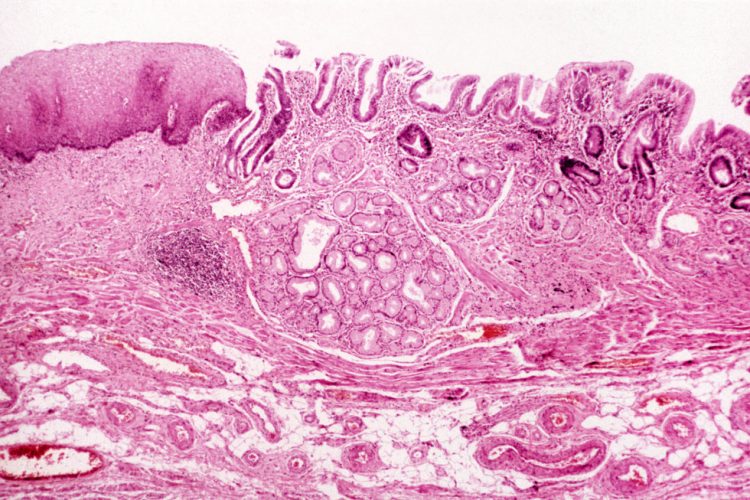
Scientists have discovered that the absence of a specific protein in cells lining the oesophagus may cause inflammation and tissue damage in people with eosinophilic esophagitis (EoE). EoE affects as many as 150,000 people in the United States, many of whom are children. People with EoE experience difficult or painful swallowing, vomiting and nutritional problems because an accumulation of immune cells called eosinophils scars the oesophagus.
The researchers found that the protein, SPINK7, was nearly absent in oesophageal biopsies taken from adults and children with active EoE but was prevalent in biopsies from healthy people. In a healthy oesophagus, SPINK7 tamps down inflammation and helps preserve tissue structure.
Encouragingly, a licensed drug for emphysema reversed damaging inflammation in tissues lacking SPINK7. The researchers received support from the National Institute of Allergy and Infectious Diseases and the National Institute of Diabetes and Digestive and Kidney Diseases, both parts of the National Institutes of Health.
Biomarkers aren’t just supporting drug discovery – they’re driving it
FREE market report
From smarter trials to faster insights, this report unpacks the science, strategy and real-world impact behind the next generation of precision therapies.
What you’ll unlock:
- How biomarkers are guiding dose selection and early efficacy decisions in complex trials
- Why multi-omics, liquid biopsy and digital tools are redefining the discovery process
- What makes lab data regulatory-ready and why alignment matters from day one
Explore how biomarkers are shaping early drug development
Access the full report – it’s free!
Because food contains enzymes that can damage human tissue, the lining of the oesophagus normally protects itself by producing its own enzymes that degrade the offending proteins and thus protect the lining. Researchers led by Dr Marc E. Rothenberg, at Cincinnati Children’s found that SPINK7 facilitates this protective process. When they silenced SPINK7, the gene that codes for SPINK7, in cells derived from oesophagal tissues, the research team discovered that large gaps formed between the cells lining the oesophagus. These cells also lost barrier functions that ordinarily move food along the digestive tract. Tissues that did not express SPINK7 also produced high levels of chemical messengers called cytokines that attract eosinophils and produce the same type of inflammation seen in allergic diseases.
The research team then treated oesophagal tissue samples with alpha-1 anti-trypsin, or A1AT, a drug approved to treat an inherited form of emphysema. Like SPINK7, A1AT is a natural inhibitor of specific tissue-damaging proteins. In the lab, A1AT reversed the damaging inflammation seen in tissues that lacked SPINK7, suggesting that further investigation is warranted to determine if this therapeutic may also benefit people with EoE.
Currently, therapies available to people with EoE include taking corticosteroids to relieve inflammatory symptoms, restricting their diets to avoid allergen-containing foods that may exacerbate the condition, or undergo periodic surgical procedures to expand the oesophagus.
The investigators report the findings in Science Translational Medicine.
Related topics
Protein, Proteomics
Related conditions
Eosinophilic esophagitis








