Intranasal drug may be the future of depression treatments
Posted: 12 November 2021 | Anna Begley (Drug Target Review) | No comments yet
Groundbreaking study succeeded in the intranasal delivery of an anti-depressant peptide-based drug to the brain in mouse models.

Researchers at the Tokyo University of Science (TUS), Japan, have achieved success in delivering the anti-depressant drug glucagon-like peptide 2 (GLP-2) in a mouse model of depression.
Previous studies working on drug delivery to the brain have been faced with several challenges. Firstly, currently used methods such as intracerebroventricular (ICV) administration are extremely invasive. Secondly, other methods such as intranasal administration face issues such as ineffective cell permeability. Thirdly, even if the drugs gain access into the neurons, their action in the brain is impeded by slow axonal transportation and fast degradation.
NEWS: Uncovering ketamine’s mechanisms helps identify depression treatment – READ HERE
“Although there have been more than 20 years of phenomenal intranasal drug delivery (IDD) research, I had wondered why it has not been put to practical use. Then, I realised that most IDD research had focused on drug delivery through the olfactory epithelium, which accounts for only 2 percent of human nasal mucosa,” explained Professor Chikamasa Yamashita who led the study. ” Alternatively, my team focused on the central delivery of drugs through the remaining 98 percent of such mucosa – respiratory epithelium, specifically through the trigeminal nerve.”
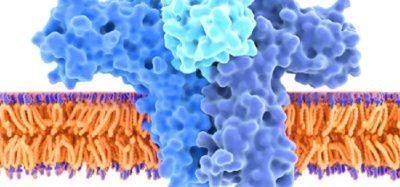
The scientists began by working with GLP-2, a neuropeptide that has shown anti-depressant effects even in treatment-resistant depression. Considering many drugs entering the body lose their therapeutic effectiveness due to endosomal degradation within the cells, the scientists added a peptide-derived sequence to GLP-2, known as a penetration accelerating sequence (PAS), to help evade this degradation. They also enhanced the permeability of the drug to the respiratory epithelium by the addition of another membrane-permeability promoting peptide-derived sequence called cell penetrating peptides (CPP). They then proceeded to test this modified drug in the mouse model of depression.
Their results, detailed in the Journal of Controlled Release, showed that GLP-2 uptake into the respiratory epithelial cells were enhanced owing to the presence of the CPP. GLP-2 endosomal escape was also enhanced by PAS. This double-modification allowed the effective nose-to-brain delivery of GLP-2. Interestingly, the researchers found that the modified IDDS achieved therapeutic effectiveness in 20 minutes, similar to ICV administration. However, IV administration did not demonstrate the intended effect.
“We hope that our results can be replicated in humans in the near future,“ concluded lead author Dr Tomomi Akit. “Our study possibly paves the way for futuristic brain delivery applications like nanobiotechnology and adult genetic engineering.”
Related topics
Drug Delivery, Drug Targets, In Vivo, Neurons, Small Molecules, Therapeutics
Related conditions
Depression
Related organisations
Tokyo University of Science
Related people
Dr Tomomi Akit, Professor Chikamasa Yamashita