Researchers delineate novel COVID-19 subgroups in critically ill patients
Posted: 6 December 2021 | Anna Begley (Drug Target Review) | No comments yet
The new study used sequence clustering analysis to identify four subgroups of COVID-19 to help match patients to specific treatments.


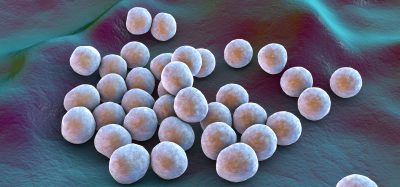
A team at Mount Sinai Hospital, US, have delineated four new subgroups of COVID-19 that can be identified in patients within 24 hours of admission to the intensive care unit (ICU). The findings will help match patients to specific treatments, improving their overall care and outcomes.
Mount Sinai researchers used sequence clustering analysis, a new data mining technique that can detect patterns of disease progression, to identify clinical subphenotypes in severely ill COVID-19 patients that had distinct temporal patterns during the first 24 hours and different clinical outcomes at 30 days. These temporal characteristics are apparent only when multiple features are considered over a period of time.
“While patients hospitalised with COVID-19 may have similar baseline characteristics, their clinical trajectories and health outcomes over time may be vastly different,” explained corresponding author Professor Girish Nadkarni. “Our study demonstrates the importance of revealing temporal similarities of diseases to identify reproducible and clinically relevant subphenotypes and suggests further exploration of the temporal progressions of these clinical features is warranted.”
The team analysed data for more than 1,000 critically ill patients with confirmed infection with SARS-CoV-2 who were admitted to the ICU. They transformed 10 biomarkers and seven treatments during the first 24 hours of the ICU admission into a sequence consisting of 16 non-overlapping interval slots, each 1.5 hours long and characterised as one of 10 distinct statuses. The results are published in JAMIA.
NEWS: Plant-derived antiviral drug could combat Delta variant
The researchers identified four COVID-19 subphenotypes using biomarkers and treatment administrations:
- Subphenotype I included patients with irregular vital signs but less need for invasive interventions within the first 24 hours. Patients in this group tended to have the highest probability of survival
- Subphenotype II represented patients with the least degree of ailments, relatively low mortality, and the highest probability of discharge from the hospital. Patients in this group were younger, more likely to be Black, less likely to need mechanical ventilation, and most likely to leave the hospital at 30 days
- Subphenotype III represented patients who experienced clinical deterioration during the first 24 hours that led to poor outcomes. Patients in this group tended to be older, were more likely male, had the highest incidence of shock at admission, and also had the highest requirement for support with shock treatment and mechanical ventilation
- Subphenotype IV represented an acute respiratory distress syndrome trajectory with an almost universal need for mechanical ventilation. This group had a relatively larger proportion of Latino patients and a high prevalence of respiratory failure; more than half were mechanically ventilated at the time of admission.
“COVID-19 has been studied extensively, yet we still have a limited understanding of effective clinical care for critically ill patients with COVID-19,” commented researcher Dr Wonsuk Oh. “State-of-the-art machine learning methods enable us to reveal novel temporal subphenotypes from one-hour resolution medical records. These temporal subphenotypes provide new insights into patients’ underlying conditions and course of disease progression during the intensive care unit stay, and ultimately facilitate personalised clinical care of patients with an informed decision.”
Related topics
Analysis, Analytical Techniques, Bioinformatics, Biomarkers, Informatics, Personalised Medicine, Sequencing, Therapeutics
Related conditions
Covid-19
Related organisations
Mount Sinai Hospital
Related people
Girish Nadkarni, Wonsuk Oh