Leukaemia-on-a-chip mimics bone marrow for better CAR T testing
Posted: 9 July 2025 | Drug Target Review | No comments yet
A new “leukaemia-on-a-chip” device replicates human bone marrow and immune interactions, enabling researchers to observe CAR T cell therapies in action – potentially allowing for more personalised treatment strategies for leukaemia patients.
Chimeric antigen receptor (CAR) T cell therapy has transformed the landscape of cancer treatment – giving patients with leukaemia and other blood cancers hope when conventional therapies fail. Yet nearly half of patients relapse and many face serious side effects – issues driven in part by the limitations of current testing methods.
Now, researchers from the Perelman School of Medicine at the University and the Tandon School of Engineering have announced a breakthrough: a miniature “leukemia-on-a-chip” device that could dramatically improve how CAR T therapies are studied and customised.
Their findings, published in Nature Biomedical Engineering, describe a first-of-its-kind platform that mimics the physical and immune environments of human bone marrow, potentially transforming both drug development and personalised treatment.
A living model of human bone marrow
The new chip-sized platform replicates three critical bone marrow regions where leukaemia originates: blood vessels, the surrounding marrow cavity and the outer bone lining. When seeded with patient bone marrow cells, the device begins to self-assemble, producing structural proteins such as collagen, fibronectin and laminin – recreating the architecture and the immune environment of human tissue.
“By mimicking the bone marrow stroma and immune niches in three dimensions, the device allows us to observe CAR T cell behaviour and efficacy in a setting that closely mirrors the complexities of a real human body,” said co-senior author Saba Ghassemi, assistant professor of pathology and laboratory medicine at Penn Medicine. “It incorporates vascular networks to support realistic immune interactions, providing a level of precision and insight that traditional 2D cell culture models or animal studies cannot achieve.”
Watching cancer treatment in action
Using advanced imaging, the researchers were able to track CAR T cells as they moved through the vascular networks, found their cancer targets and attacked them – revealing processes that were previously invisible.
“We observed immune cells patrolling their environment, making contact with cancer cells, and killing them one by one,” said co-senior author Weiqiang Chen, professor at NYU Tandon.
The team noticed that CAR T cells moved quickly while searching for cancer but slowed when they detected a target, increasing precision in their attack. The platform also revealed a “bystander effect,” where engineered immune cells activated others nearby, potentially enhancing efficacy but also contributing to side effects.
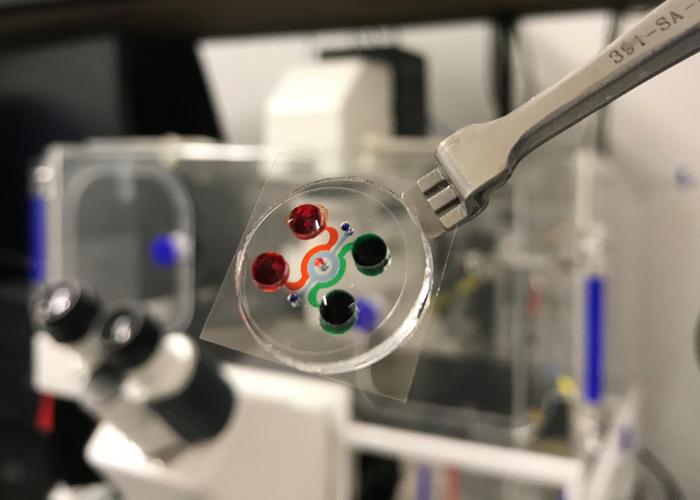
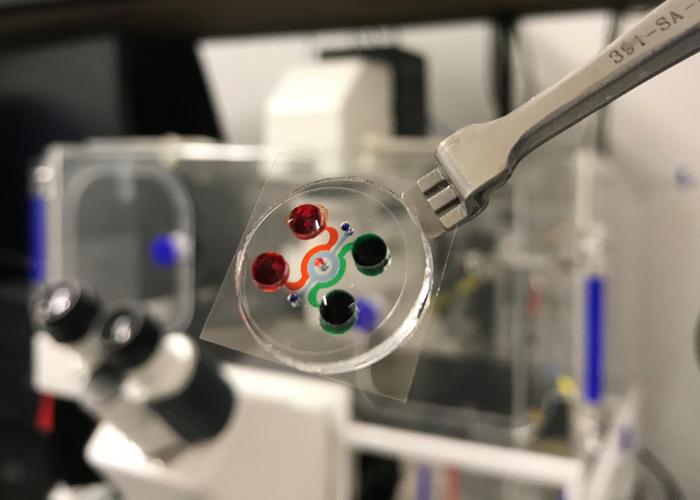
The actual chip of human leukaemia bone marrow where chambers and channels were filled with food dyes. Credit: NYU Tandon Applied Micro-Bioengineering Laboratory/Courtesy of Weiqiang Chen.
Simulating real patient scenarios
Researchers were able to manipulate the device to simulate various clinical outcomes -complete remission, treatment resistance and relapse. Tests showed that newer “fourth generation” CAR T cells, designed with improved features, outperformed older versions, particularly at lower doses.
“This device addresses a significant gap in preclinical research, offering an advanced tool for studying CAR T cell therapy’s dynamic and multifaceted responses to leukaemia,” Ghassemi said. “Its ability to model these processes in real time opens the door for more accurate predictions of clinical outcomes, ultimately helping to refine treatments before they are tested in patients.”
Faster, ethical and more personalised testing
With the ability to be assembled in under a day and run experiments in just two weeks, the leukaemia-on-a-chip offers major time and ethical advantages over animal models – which can take months to prepare.
“We can now watch cancer treatments unfold as they would in a patient, but under completely controlled conditions without animal experimentation,” Chen noted.
The timing is also significant, aligning with the US FDA’s recent roadmap to reduce reliance on animal testing for drug development.
Related topics
Assays, Bioengineering, Cancer research, Cell Therapy, Chimeric Antigen Receptors (CARs), Drug Discovery Processes, Imaging, Immunotherapy, In Vitro, Organ-on-a-Chip, Precision Medicine, T cells, Translational Science
Related conditions
blood cancer, Leukaemia
Related organisations
the Perelman School of Medicine at the University, the Tandon School of Engineering