Challenges in developing robust potency assays for ADCs
Posted: 18 August 2025 | Drug Target Review | No comments yet
Developing robust potency assays for Antibody-Drug Conjugates (ADCs) is crucial for ensuring their clinical success, but designing assays that meet both technical and regulatory standards is challenging. Here, Abzena’s CSO Campbell Bunce explores the complexities of assay development and the importance of ensuring accuracy, consistency and regulatory alignment for ADCs to reach their potential.
A key to the success of any Antibody-Drug Conjugate (ADC) program is having an appropriate and robust potency assay, as without precise testing, even the most promising drug can fail to meet regulatory standards and never reach patients. Unlike standard biologics, ADCs require potency assays that assess both targeted binding and cytotoxic impact, which adds complexity to assay design and validation. Cell-based potency assays, widely used in ADC testing, must evolve from early research models into validated methods that meet a range of regulatory expectations. However, designing these assays is no straightforward task.
Importance of potency assays in ADC development
Potency assays are in vitro bioassays that measure the functional effect of an ADC on the target system to confirm its biological activity. These assays quantify cytotoxic effects by assessing cell viability, apoptosis or proliferation inhibition after ADC exposure. Regulatory agencies also mandate validated potency assays for drug release and stability testing and expect ongoing batch-to-batch consistency. Furthermore, potency assays can also be an integral part of any extended characterisation study and other development studies.
ADCs present additional complexity due to their highly cytotoxic payloads. Assays must reliably quantify potency at sub-nanomolar concentrations while minimising variability.
ADCs present additional complexity due to their highly cytotoxic payloads. Assays must reliably quantify potency at sub-nanomolar concentrations while minimising variability. However, even small changes in cell culture conditions, passage number, or reagent consistency and stability can affect these results. To maintain consistency, developers rely on reference standards, extensive statistical analyses, defined acceptance criteria and well- controls to ensure the reliability and accuracy of the potency assays across different batches and testing conditions.
Biomarkers are redefining how precision therapies are discovered, validated and delivered.
This exclusive expert-led report reveals how leading teams are using biomarker science to drive faster insights, cleaner data and more targeted treatments – from discovery to diagnostics.
Inside the report:
- How leading organisations are reshaping strategy with biomarker-led approaches
- Better tools for real-time decision-making – turning complex data into faster insights
- Global standardisation and assay sensitivity – what it takes to scale across networks
Discover how biomarker science is addressing the biggest hurdles in drug discovery, translational research and precision medicine – access your free copy today
Different ADCs may require different potency assays depending on their mechanism-of-action (MoA). For cytotoxic ADCs, endpoint viability or apoptosis assays provide the most direct potency measurement. ADCs with immune-modulatory activity may require additional assays, such as Fc effector function or reporter gene assays.
Regulators require potency assays to catch changes in drug activity caused by variables in ADC properties like linker-payload conjugation, glycosylation or aggregation between batches.
Regulatory guidelines also have their own sets of strict validation criteria. The US Food and Drug Administration (FDA) requires MoA-reflective functional assays for lot release, while the European Medicines Agency (EMA) may accept surrogate assays under specific conditions. Potency assays must comply with current good manufacturing practice (cGMP) regulations and International Council for Harmonisation (ICH) Guideline Q2 (R2), which cover accuracy, precision, specificity, and linearity.
Regulators require potency assays to catch changes in drug activity caused by variables in ADC properties like linker-payload conjugation, glycosylation or aggregation between batches. A well-characterised potency assay will differentiate between an active and inactive drug to ensure accurate interpretation of stability data.
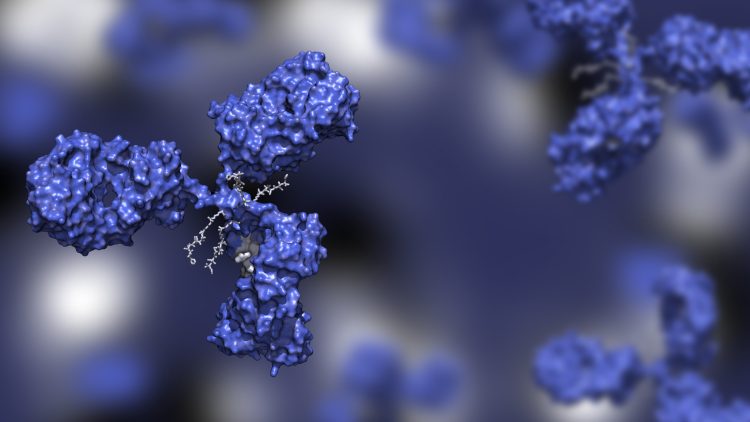
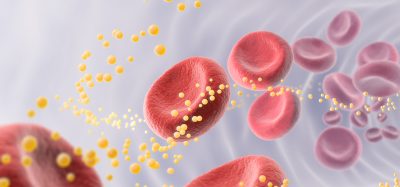
Antibody–Drug Conjugate (ADC): A targeted cancer therapy that combines an antibody (to seek out specific cancer cells) with a potent drug payload (to destroy them), aiming to maximise tumour kill while sparing healthy tissue. Image credit: Huen Structure Bio / Shutterstock
Technical challenges in developing cell-based assays
Getting ADC potency assays right is far from easy – the inherent variability in biological systems makes precision and reproducibility challenging, especially in cell-based models. A suitable cell model must express the target antigen at physiologically relevant levels and respond consistently to the ADC’s MoA. Variability in receptor density, intracellular trafficking, and metabolic activity can alter assay performance and throw data reliability into question.
Developers need to have tight control of assay conditions. Passage number, media composition and incubation time influence cell viability and drug response, while inconsistencies in serum batches or enzyme activity during cell detachment can introduce variability.
Developers need to have tight control of assay conditions. Passage number, media composition and incubation time influence cell viability and drug response, while inconsistencies in serum batches or enzyme activity during cell detachment can introduce variability. Standardised protocols and well-characterised cell banks are therefore essential to help maintain assay stability.
Signal-to-noise ratio is a key challenge in ADC potency assays. Achieving a suitably large assay window requires sensitive detection methods, but excessive amplification increases background noise. Optimising parameters such as cell density, incubation time and detection reagents will produce a reliable dynamic range.
Moving from early-phase assays to GMP-compliant methods further necessitates additional requirements. Any potency assay must meet regulatory criteria for accuracy, linearity, specificity and precision, while maintaining sufficient throughput for batch testing. Parallelism assessments help confirm that test samples behave consistently with reference standards, and statistical modeling – such as dose-response curve fitting and outlier analysis – strengthens data reliability.
Cross-site reproducibility adds another layer of complexity, as assays must deliver consistent results across different laboratories, operators and instruments. Early harmonisation of protocols and multi-site validation, therefore, reduces variability and supports a smoother transition from R&D to commercial manufacturing. It is also essential to generate sufficient data before initiating formal validation activities to establish the most appropriate validation criteria and confirm the assay is fit-for-purpose. Furthermore, as ADC programs progress towards commercialisation, identifying and managing critical reagents for potency becomes pivotal. Once identified, these critical reagents must undergo the necessary qualification –based on the specific needs – to ensure consistent and reliable assay performance across the product lifecycle.
Bridging the gap between R&D and regulatory requirements
Regulatory agencies set strict potency assay requirements to confirm an ADC’s quality, safety and consistency. Early-stage research assays often lack the reproducibility and specificity required for lot release. It is imperative that developers refine their assay design, demonstrate consistent performance across multiple runs and establish well-defined acceptance criteria to meet regulatory requirements.
MoA-reflective potency assays with robust validation data help reduce the risk of regulatory delays. Regulators expect clear justification for the selection of assays, validation criteria and statistical models used in testing. Regulatory interactions during preclinical and early clinical phases help ensure that potency assays align with expectations – this can minimise later-stage modifications that could otherwise complicate approval.
An experienced contract development and manufacturing organisation (CDMO) can help with regulatory submissions by aligning potency assay strategies with regulatory expectations.
An experienced contract development and manufacturing organisation (CDMO) can help with regulatory submissions by aligning potency assay strategies with regulatory expectations. They have teams to assist with compiling potency assay validation data for Investigational New Drug (IND) and Biologics License Applications (BLAs), so that documentation meets FDA and EMA standards. Abzena uses a phase-appropriate approach to help developers transition from early exploratory assays to fully validated, GMP-compliant potency testing to reduce the risk of regulatory delays.
Operational consistency presents another challenge. Assay performance can vary due to differences in equipment calibration, operator technique, or environmental conditions. A good CDMO will employ cross-site validation to ensure assays are harmonized between different facilities – this makes for consistent data generation across different sites. Early collaboration between research, quality control (QC) and regulatory teams improves the likelihood of a smooth transition from development to commercial manufacturing.
Handling highly cytotoxic material in ADC testing
ADCs contain highly cytotoxic payloads that need strict handling procedures to protect personnel and maintain data integrity. Even at picomolar concentrations, these compounds present risks during assay execution. Laboratories that run ADC potency assays must implement controlled environments, specialised containment systems and rigorous safety protocols.
Personnel must wear double gloves, respiratory protection and disposable gowns to prevent exposure. Controlled workflows and validated decontamination procedures should be in place to minimise cross-contamination between test samples, reference standards and controls.
Stability testing is essential for accurate potency measurements, as ADCs degrade under improper storage conditions, which affects assay results.
Stability testing is essential for accurate potency measurements, as ADCs degrade under improper storage conditions, which affects assay results. Stability studies assess degradation profiles under different temperatures, humidity levels and freeze-thaw cycles. Testing laboratories must therefore track these parameters to prevent artefactual potency shifts.
Disposing of ADC-contaminated materials presents additional challenges, as used culture plates, pipette tips and media all require specific levels of decontamination before disposal. Chemical inactivation, autoclaving and incineration are methods used to eliminate residual cytotoxicity, and facilities must comply with local and international regulations governing hazardous biological waste.
Analysts handling ADC assays must also undergo biosafety training that covers cytotoxic handling, emergency response and assay-specific risk assessments. Routine audits reinforce compliance and identify areas for process improvement.
Specialised testing facilities and advanced analytical techniques
ADC potency assays require controlled environments, validated methods and specialised expertise to generate reliable data for regulatory approval. These specialised testing facilities reduce the risks associated with variability, assay transfer and sample integrity.
Advanced and appropriate analytical technologies will enhance ADC research and development from the start. High-throughput screening platforms automate sample handling and data acquisition, which increases assay efficiency and reduces manual variability. Automated liquid handling systems improve assay reproducibility by minimising human error in sample preparation. These systems ensure consistent dosing, reduce variability, and streamline high-throughput potency testing, which is especially important in the lead selection phase.
Other advanced analytical capabilities, such as live-cell imaging techniques, enable the real-time tracking of ADC-induced cytotoxic effects, providing dynamic insights into cell viability and apoptosis beyond traditional endpoint assays. The support of microscopy techniques can improve lead selection by capturing cellular responses in real-time and helping detect subtle potency differences that standard plate-reader assays might miss. Such detailed characterisation of the MoA can provide invaluable data for potency assay design to ensure that the best cell system and readout are chosen.
By combining specialised expertise with advanced analytical platforms, developers and CDMOs can improve ADC potency testing beyond traditional methods. Working with a dedicated testing facility from the outset will help align assay design with regulatory and manufacturing requirements, which avoids many potential delays and supports commercial readiness.
Accuracy and precision in potency
Potency assay development for ADCs requires technical precision, regulatory compliance and strict quality control. Assays must generate reliable, batch-consistent data while detecting subtle potency shifts. The transition from early-phase methods to GMP-validated assays involves extensive statistical evaluation, performance trending, and regulatory oversight.
ADCs present unique challenges due to their cytotoxic payloads and complex MoAs. Assay design must account for biological variability, reagent stability and site-to-site reproducibility, while regulatory agencies require MoA-reflective assays with clear validation data.
As ADCs become more complex, so must the assays that define their potency – accuracy, precision, adaptability and early regulatory alignment will separate success from failure.
Meet the expert
Campbell Bunce 

Campbell has over 25 years of experience working in the biotech and diagnostics sectors. Before joining Abzena in 2015, he held multiple positions of increasing responsibility in biotech, including Head of Cellular Immunology at Cantab Pharmaceuticals, Director of Programs at Piramed Pharma, and R&D Director at Immune Targeting systems.
Throughout his career he has applied innovative solutions for the design, manufacture and clinical evaluation of novel products including vaccines, biologics and small molecules in multiple therapeutic areas. These include inflammation, cancer, infectious disease and addiction. Campbell has a PhD in immunology from the University of Manchester, an Executive MBA from Judge Business School, Cambridge University and has published a number of papers on cell-mediated immunity, immunotherapy and vaccines.
Related topics
Affimers, Analysis, Analytical Techniques, Antibodies, Assays, Biologics, Biopharmaceuticals, Cancer research, cytotoxicity, Cytotoxicity assays, Immuno-oncology, Immunotherapy, Oncology, Therapeutics
Related conditions
Cancer
Related organisations
Abzena