PDX models are back – and they’re exposing what cell lines missed
Posted: 22 September 2025 | Drug Target Review | No comments yet
As cancer drugs continue to fail in translation, researchers are turning back to patient-derived xenograft (PDX) models – this time with better science. Could they be the missing link between the lab and the clinic?


As precision medicine continues to be a central strategy in cancer treatment, a key challenge remains: how can drugs be better matched with patients before they enter clinical trials? For Dr Michael J. Wick, Chief Scientific Officer at The START Center for Cancer Research and co-founder of its pre-clinical division XenoSTART, the answer lies in a decades-old modality now being redefined for modern oncology – patient-derived xenografts (PDX).
With a background in chemistry, biochemistry and molecular pharmacology, Wick has spent nearly three decades at the heart of translational oncology. After co-founding XenoSTART in 2007, he has dedicated his work to building a highly differentiated, diverse and clinically reflective PDX platform that has become instrumental in helping pharmaceutical and biotech companies de-risk early drug development.
“We need to be able to interact with and access patients at every stage of disease – to help pharmaceutical and biotech companies really match their drug with the patient population that’s going to be using it, both in trials and once the drug is approved,” shares Wick.
Biomarkers are redefining how precision therapies are discovered, validated and delivered.
This exclusive expert-led report reveals how leading teams are using biomarker science to drive faster insights, cleaner data and more targeted treatments – from discovery to diagnostics.
Inside the report:
- How leading organisations are reshaping strategy with biomarker-led approaches
- Better tools for real-time decision-making – turning complex data into faster insights
- Global standardisation and assay sensitivity – what it takes to scale across networks
Discover how biomarker science is addressing the biggest hurdles in drug discovery, translational research and precision medicine – access your free copy today
Why traditional models were not enough
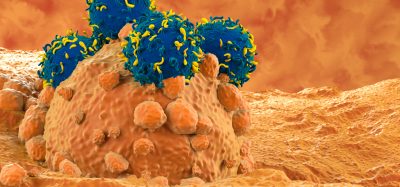
PDX are not new. These models are developed by implanting tumour samples directly from a cancer patient into an immunodeficient mouse, enabling the tumour to grow in a living system and preserving the biological characteristics of the original cancer. PDX models have been part of the cancer research toolbox for decades. However, in the 1980s, the industry shifted its focus towards cancer cell lines – standardised, scalable and easy to use. The problem? They were too simple.
“The material – the cell lines that were being used – really took away a lot of the ‘human’ of the cancer,” says Wick.
By immortalising and repeatedly passaging these cells, researchers created stable models – but ones increasingly detached from the complexity of human tumours. As a result, drugs that performed well in vitro and resulting cell-derived xenografts (CDX) models, often failed once tested in the clinic.
You really need to test a broader population of models representing specific cancer types…or you may slow down the disease, but you do not eliminate it – and basically just delay the inevitable.
That gap highlighted the limitations of traditional CDX models and prompted a renewed focus on PDX – this time with an emphasis on reflecting patient biology and clinical treatment history. At XenoSTART, that has meant developing models from patient tumours across all stages of disease; prioritising pretreated, heterogeneous and ethnically diverse samples.
“You really need to test a broader population of models representing specific cancer types…or you may slow down the disease, but you do not eliminate it – and basically just delay the inevitable.”
Breast cancer: building the world’s largest ER+ PDX platform
Among their 3,000+ PDX models, XenoSTART holds one of the largest collections of oestrogen receptor-positive (ER+) breast cancer models worldwide. ER+ tumours are a subtype of breast cancer in which tumour growth is driven by the hormone oestrogen. These models are particularly valuable as ER+ breast cancers represent the majority of breast cancer cases yet can respond very differently depending on patient treatment history and hormone sensitivity.
XenoSTART’s collection spans the full clinical spectrum – from treatment-naïve to heavily pretreated – and includes patients from a wide range of ethnic backgrounds.
Why does this matter? ER+ breast tumour modelling is notoriously difficult to establish in vivo, particularly from treatment-naïve patients. By refining their development process early, Wick and his team were able to overcome this challenge ahead of most other groups.
This platform also reflects recent FDA guidance encouraging drug developers to ensure their preclinical studies account for patient diversity. Wick views this as both a scientific and ethical imperative – and one that XenoSTART is particularly well positioned to address.
From San Antonio to Madrid
XenoSTART’s reach is rapidly expanding. Its original base in San Antonio gave them access to a broad patient population in South Texas, and they have since added sites in Michigan and two in Madrid, Spain.
“Having access to patient populations that are diverse… being able to collect samples and make models from patients with different genetic backgrounds is and will continue to be incredibly powerful in the future.”
Studies have shown that ethnic variations can significantly affect how patients respond to therapies. By integrating genetic diversity into preclinical research, Wick and his team aim to predict those differences before a drug ever reaches the clinic.
How PDX is accelerating drug timelines
Wick is the first to acknowledge that building an extensive PDX platform is not just about collecting samples – it is about translating them into actionable insights.
They utilised our panel of E17K-mutant models and were able to move into clinical trials five to six times faster than they would’ve been able to without this resource.
One standout example involves a collaborator developing a novel AKT1 inhibitor targeting the E17K mutation – an alteration linked to breast and other cancer types. Previous AKT inhibitors had shown preclinical activity but were limited by toxicity, particularly hyperglycaemia. This new compound, however, showed promise.
“They utilised our panel of E17K-mutant models and were able to move into clinical trials five to six times faster than they would’ve been able to without this resource,” Wick says.
Since XenoSTART had multiple models with that precise mutation, the collaborator was able to validate its therapy quickly and move into clinical trials in several tumour types and with a higher degree of confidence.
Other collaborations have similarly used the XenoSTART PDX library to match drug candidates with the exact patient populations they aim to treat. In each case, real-world biology has made for better bench-to-bedside predictions.
Translational research in action
A recurring theme in Wick’s work is translational relevance. With over 3,000 models and counting, XenoSTART’s focus is not only on testing novel drugs but also testing approved therapies across alternate cancer types to try and find new sensitive indications.
“Whenever a patient progresses on a therapy, there may or may not be another drug available for them… having models that represent those patients allows these next generation therapies to be validated.”
Most of XenoSTART’s PDX models are established from patients who have progressed on various lines of therapy, providing a more clinically relevant context for evaluating new treatments. These models more accurately maintain the original tumour microenvironment, preserving key biological features.
Fusion genes and ADCs
Looking ahead, Wick is particularly excited by two trends shaping future oncology R&D: antibody–drug conjugates (ADCs) and gene fusions.
On the gene fusion side, XenoSTART and its collaborators have identified novel fusion drivers not only in rare cancers but also in higher-incidence types such as breast and lung. These fusions – previously overlooked – are now emerging as prime targets for next-generation therapies.
Gene fusion drivers are really where the next 10 to 15 years are going to be exciting… new targets for drugs to go after.
“Gene fusion drivers are really where the next 10 to 15 years are going to be exciting… new targets for drugs to go after,” Wick enthuses.
ADCs have also gained significant traction. While earlier generations were limited by unstable linkers and off-target toxicity, newer ADCs have demonstrated strong clinical efficacy. Wick sees growing potential not only in toxin-linked ADCs, but also in radiotherapy-based conjugates, bispecific formats and those incorporating kinase inhibitors.
“The flexibility for these targeting therapies across different indications is a hallmark and a really exciting opportunity,” says Wick.
The role of patients and clinicians
For all the cutting-edge science, Wick remains grounded in the human element behind the models. None of XenoSTART’s work would be possible, he emphasises, without the patients who agree to share their samples and the clinical investigators who help guide the science.
“Without their commitment and input, we could do well, but we would not be successful,” he finishes.
As XenoSTART expands its footprint and accelerates oncology drug development, it is clear that its model – both scientifically and operationally – is working. It is not just about building better mice. It is about building better medicines, faster and for everyone.
Meet the expert


Dr Michael J. Wick is Chief Scientific Officer of The START Center for Cancer Research and co-founder of its preclinical division, XenoSTART. He is internationally recognised in the field of preclinical oncology drug development, with a career spanning more than 30 years, and is considered one of the foremost experts in establishing clinically relevant animal models of human cancer.
Under Dr Wick’s leadership, XenoSTART has grown to become one of the world’s largest providers of patient-derived xenograft (PDX) models, with a portfolio of more than 3,000 models across 30+ cancer indications, including the most extensive available panel of breast cancer PDX models.
Before founding XenoSTART, Dr Wick served as Director of Preclinical Research at the Cancer Therapy & Research Center’s Institute for Drug Development, where he was instrumental in re-establishing PDX models as a cornerstone of preclinical oncology research.
He earned his PhD in molecular pharmacology from The University of Texas Health Science Center at San Antonio, followed by an NCI postdoctoral fellowship at the University of North Carolina at Chapel Hill. He also holds dual Bachelor of Science degrees in chemistry and biochemistry from The University of Texas at Austin, and is currently Adjunct Assistant Professor in the Department of Pharmacology at The University of Texas Health Science Center at San Antonio.
Related topics
Analysis, Animal Models, Antibodies, Cancer research, Cell Line Development, Drug Delivery, Drug Development, Kinases, Molecular Biology
Related conditions
Breast cancer, Lung cancer
Related organisations
The START Center for Cancer Research, XenoSTART