New drug boosts foetal haemoglobin to fight sickle cell disease
Posted: 18 May 2023 | Tony Portelli (Drug Target Review) | No comments yet
Researchers are exploring the potential use of HDAC inhibitors, a group of drugs known for their capability to impede tumour cell division, to reduce the pain and damage associated with sickle cell disease. The drugs have shown initial evidence of reactivating the gene responsible for producing foetal haemoglobin, which cannot undergo sickling after birth.
Results of the Multicenter Study of Hydroxyurea in Sickle Cell Anaemia published in the Journal of the American Medical Association in 2003, indicated that the use of hydroxyurea, the only drug approved at the time, reduced mortality as it reduced pain crises and increased foetal haemoglobin. Foetal haemoglobin (HbF) is the predominant type of haemoglobin (Hb) in foetal life and remains so until just before birth when its production is turned down while the production of adult Hb is turned up. 1
According to Abdullah Kutlar, MD, who serves as the director of the Center for Blood Disorders at the Medical College of Georgia and Augusta University Health, these drugs, referred to as HDAC inhibitors, have shown initial evidence of reactivating the gene responsible for producing foetal haemoglobin, which cannot undergo sickling after birth. One such drug, Panobinostat, has been singled out for further investigation.
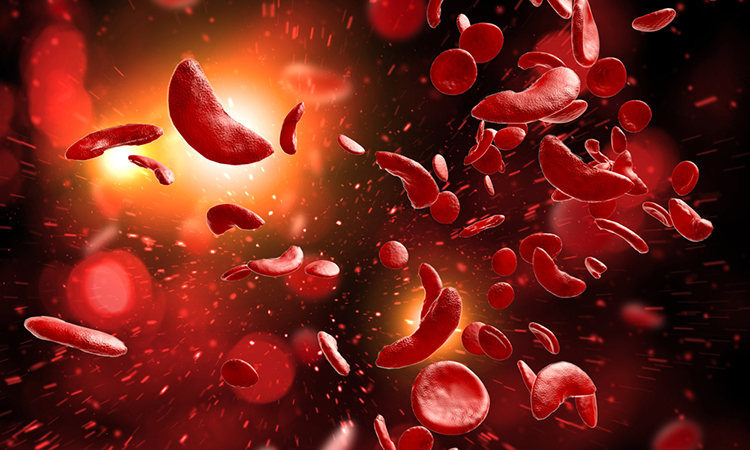
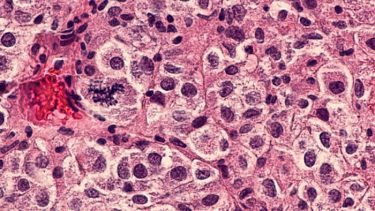
The red blood cells contain haemoglobin, which plays a crucial role in transporting oxygen throughout the body. In sickle cell disease, however, this function is impaired, leading to a range of potential health consequences. The irregularly shaped and sticky red blood cells produced by the disease can obstruct small blood vessels, causing recurring painful attacks. Additionally, patients often experience haemolysis, or rapid breakdown, of their red blood cells, which can lead to anaemia, damage to vital organs, and a reduced lifespan.
Histone deacetylases (HDACs) are a type of enzyme that plays a role in reducing the expression of certain genes, including the gamma-globin gene responsible for the production of foetal haemoglobin. This is a natural process that occurs as we transition from childhood to adulthood. Foetal haemoglobin is critical for developing babies as it allows them to extract oxygen from the mother’s blood, while adult haemoglobin, produced by the beta-globin gene, carries oxygen. However, within a few months after birth, the levels of foetal haemoglobin significantly decrease and are replaced by adult haemoglobin.
Abdullah Kutlar and Betty Pace, MD, a sickle cell researcher and Francis J. Tedesco Distinguished Chair of Paediatric Haematology and Oncology, are collaborating as co-principal investigators on a new clinical trial, which has been awarded a $2.3 million grant from the National Heart, Lung and Blood Institute. The three-year study aims to investigate the potential of the HDAC inhibitor Panobinostat to reactivate the foetal haemoglobin gene in adults, addressing the root cause of inefficient oxygen delivery. The trial represents an early-stage effort to determine the viability of this approach.
“HDAC inhibitors are drugs known to change the expression of certain genes,” says Kutlar. “When you inhibit the histone deacetylases, what you do is enable some of the genes that have been shut down by certain mechanisms to get expressed again. That is important for sickle cell because we know in adults that the foetal haemoglobin gene is shut down and we know foetal haemoglobin works very well as a disease modifier.”
The silencing of the foetal haemoglobin gene involves two HDACs, and Panobinostat is a pan-HDAC inhibitor that targets multiple HDACs. Hydroxyurea, the first sickle cell drug approved by the U.S. Food and Drug Administration in 1998, is also known to increase foetal haemoglobin levels, although the exact mechanism behind this effect is still unknown. Additionally, hydroxyurea is used to treat certain types of cancer. According to Kutlar, if Panobinostat shows continued promise in clinical trials, the next steps will involve investigating the potential synergistic effects of combining the two foetal haemoglobin promoters.
The investigators will collaborate with study participants to identify effective strategies for adhering to the medication regimen during the trial and beyond. They will also investigate biomarkers that may indicate the suitability of the treatment for individual patients. Specifically, the study will assess the effects of Panobinostat on non-histone proteins such as NFkB, a regulator of innate immunity, and p53, a protein that plays a critical role in controlling cell division and apoptosis. In addition to histones, which are crucial for gene regulation, these non-histone proteins will be examined to gain a more comprehensive understanding of the drug’s mechanism of action.
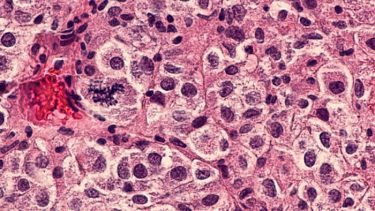
The investigators have obtained preliminary evidence that Panobinostat, administered orally in pill form, could directly address the haemoglobin dysfunction in sickle cell disease. Betty Pace has demonstrated that Panobinostat can increase foetal haemoglobin expression both in red blood cells grown in culture and in mouse models of sickle cell disease by reactivating the foetal haemoglobin gene. In an early, small-scale trial conducted by Kutlar, administering 10 milligrams of the drug to patients resulted in a slight increase in foetal haemoglobin levels, and the drug was well tolerated.
To ensure that the observed increase in foetal haemoglobin levels is due to Panobinostat and not hydroxyurea, Kutlar will focus on patients with sickle cell disease who are not taking hydroxyurea for this clinical trial. He expects that most participants will be drawn from the pool of approximately 120 patients currently being treated at the Center for Blood Disorders, many of whom have declined hydroxyurea therapy.
Kutlar and his colleagues report that long-term use of hydroxyurea has been associated with side effects such as decreased fertility in males, increased risk of skin cancer and leukaemia, and weight gain. Consequently, some patients decline to use the drug, underscoring the need for additional treatment options.
Kutlar says the possibilities of this additional therapy are exciting. “It’s not going to be a cure for sickle cell disease but it’s going to be a significant disease modifier, which will let these patients survive longer without so much organ damage and hopefully without so much pain,” he says.
Kutlar notes that bone marrow transplants are considered curative for sickle cell disease, and gene therapies such as CRISPR to increase foetal haemoglobin expression or repair the genetic cause of the disease are also under study. While these approaches show promise, additional medications are still required because it may take many years, if ever, before these sophisticated techniques are widely accessible in regions where sickle cell disease is most prevalent, such as Africa or India. Additionally, not all patients respond to every drug.
L-glutamine (Endari), which was approved by the FDA in 2017, is one of the three drugs currently available for sickle cell disease. It helps safeguard red blood cells from damage. The other two drugs, monoclonal antibody crizanlizumab (Adakevo) and voxelotor (Oxbryta), were both approved in 2019. Crizanlizumab aids in preventing red blood cells from sticking to blood vessel walls, while voxelotor helps prevent sickling and promotes better oxygen transport.
The Medical College of Georgia (MCG) participated in the clinical trials for hydroxyurea and was the largest enroller for participants in the crizanlizumab studies.
Panobinostat (Farydak) has already been used in the US for treating multiple myeloma and is still being used in Europe for the same purpose. The drug has also been studied as a possible cure for HIV infection, indicating that there is significant human experience with the drug. Kutlar points out that some adults with naturally high foetal haemoglobin levels are sickle cell resistant, providing further evidence that drugs that increase those levels can be beneficial in treating sickle cell disease.
MCG, AU Medical Center and Children’s Hospital of Georgia follow about 1,500 patients, including both adults and children, who have sickle cell disease. According to the Centers for Disease Control and Prevention, sickle cell disease affects approximately 100,000 people in the US and is most prevalent in individuals whose ancestors came from sub-Saharan Africa, Spanish-speaking regions in the Western Hemisphere, Saudi Arabia, India and Mediterranean countries such as Turkey and Greece. In Georgia alone, about 150 babies are born each year with sickle cell disease, and approximately 3,000 are born throughout the US.
References
- Lay Thein S [Internet]. [cited 2023 May 11]. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/j.1365-2141.2009.07650.x
Related topics
Cell Therapy, CRISPR, Drug Discovery, Drug Targets, Gene Therapy, Genome Editing, Targets
Related conditions
sickle cell disease
Related organisations
Augusta University Health, Medical College of Georgia
Related people
Abdullah Kutlar, Betty Pace