Stem cell therapy: Alzheimer’s disease symptoms
Posted: 31 August 2023 | Tony Portelli (Drug Target Review) | No comments yet
In the pursuit of a remedy for Alzheimer’s disease, a frontier in medical science is illuminating a glimmer of hope. Stem cell therapies have already demonstrated their prowess in treating diverse cancers and ailments linked to the blood and immune system.
In the pursuit of a remedy for Alzheimer’s disease, a frontier in medical science is illuminating a glimmer of hope. Stem cell therapies have already demonstrated their prowess in treating diverse cancers and ailments linked to the blood and immune system. In an innovative proof-of-concept investigation, researchers at the University of California San Diego have revealed the potential of stem cell transplants as a promising therapeutic avenue against Alzheimer’s disease.
The outcomes of this study, which is published in Cell Reports, present compelling evidence that the transplantation of hematopoietic stem and progenitor cells could hold the key to mitigating multiple aspects of Alzheimer’s disease in a mouse model. Mice that underwent transplantation with healthy hematopoietic stem cells exhibited not only preserved memory and cognitive function but also a marked reduction in neuroinflammation and a substantial decline in β-amyloid accumulation, a hallmark of Alzheimer’s pathology.
Dr Stephanie Cherqui, the senior author of the study and a professor at UC San Diego School of Medicine, remarked on the intricacy of Alzheimer’s disease and the necessity for treatments to address its multifaceted biological underpinnings. She noted that their research highlights the potential of hematopoietic stem and progenitor cell transplantation to thwart complications arising from Alzheimer’s, raising the prospect of an innovative therapeutic intervention for this debilitating disorder.
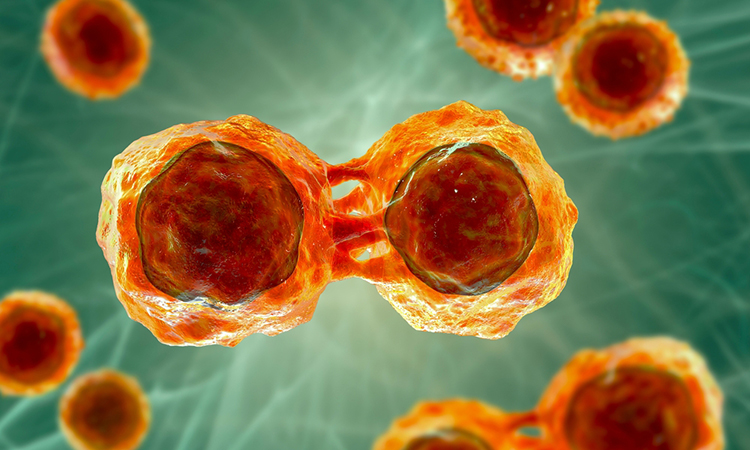
The success of this therapeutic approach hinges on its impact on microglia, a specialised type of immune cell residing in the brain. Microglia play intricate roles in the initiation and progression of Alzheimer’s through various mechanisms. Chronic inflammation involving microglia has been linked to the disease, as the release of inflammatory molecules triggers an increase in β-amyloid production. Under normal conditions, microglia play a pivotal role in eliminating β-amyloid plaques, but this function is impaired in Alzheimer’s disease. Consequently, the accumulation of β-amyloid not only exerts stress on other brain cells but also affects endothelial cells responsible for regulating cerebral blood flow.
Dr Priyanka Mishra, the lead author of the study and a postdoctoral researcher, embarked on an endeavour to ascertain whether stem cell transplants could yield a fresh population of healthy microglia capable of attenuating the progression of Alzheimer’s disease. Building upon previous successes with stem cell transplants in treating mouse models of other diseases, the research team conducted systemic transplantations of healthy hematopoietic stem and progenitor cells into mice afflicted with Alzheimer’s.
The results of their experiment were nothing short of promising. The transplanted stem cells effectively differentiated into microglia-like cells within the brain. More importantly, behavioural assessments of the mice revealed that memory loss and cognitive impairment were altogether prevented in those that received the stem cell transplant. These mice exhibited improved object recognition, normal anxiety levels, and unimpaired locomotor activity compared to untreated Alzheimer’s mice.
Upon further examination of the brain tissue, the researchers observed a significant reduction in β-amyloid plaques in the hippocampus and cortex of mice treated with healthy stem cells. Additionally, the transplantation led to diminished microgliosis, a hallmark of neuroinflammation, and aided in upholding the integrity of the blood-brain barrier.
Further insights were garnered through transcriptomic analyses, uncovering alterations in gene expression in treated versus untreated Alzheimer’s mice. The mice that underwent stem cell therapy displayed lower cortical expression of genes associated with compromised microglia and reduced hippocampal expression of genes linked to impaired endothelial cells.
Collectively, the transplantation of robust hematopoietic stem and progenitor cells orchestrated improvements in microglial health, thereby conferring protection against various facets of Alzheimer’s pathology. Notably, a third group of mice that received stem cells from Alzheimer’s-afflicted counterparts exhibited no signs of improvement, underscoring that these cells retained the disease-related traits associated with Alzheimer’s.
Moving forward, the investigation will delve into the intricate mechanisms underpinning the substantial enhancements observed and explore the potential of employing analogous transplant strategies to ameliorate Alzheimer’s symptoms in human subjects.
In light of the profound emotional and economic burdens imposed by Alzheimer’s disease on society, Dr Cherqui underscored the significance of these promising preclinical outcomes. She expressed enthusiasm for the prospect of leveraging hematopoietic stem cell therapy to devise an innovative therapeutic approach for this devastating disorder. As the search for an effective treatment marches on, stem cell therapy emerges as a beacon of hope on the horizon of Alzheimer’s research.
Related topics
Stem Cells, Targets
Related organisations
University of California San Diego