Biological robots: a new therapeutic tool
Posted: 9 January 2024 | Ellen Capon (Drug Target Review) | No comments yet
Anthrobots derived from human tracheal cells could perform therapeutic work without initiating an immune response.
Tiny biological robots have been created by scientists at Tufts University and Harvard University’s Wyss Institute. Named ‘anthrobots,’ they are derived from human tracheal cells and can move across a surface. Ranging in size, they can self-assemble and have a profound healing effect on other cells.
Prior to the new study, the laboratories of Dr Michael Levin, Vannevar Bush Professor of Biology at Tufts University School of Arts & Sciences, and Dr Josh Bongard at the University of Vermont, created multicellular biological robots from frog embryo cells, named xenobots. These could navigate passageways, collect material, record information, heal themselves from injury and replicate for a few cycles by themselves. However, it was unclear whether these capabilities were dependent on being made from an amphibian embryo, or if biobots could be constructed from other species’ cells.
The current work by Dr Levin and PhD student Gizem Gumuskaya found that bots can be created from adult human cells without the requirement for genetic modification, and more capabilities were observed in these bots compared to the xenobots. This discovery begins to solve a wider question posed by the lab: what governs how cells assemble and work together in the body, and can the cells be taken out of their natural context and recombined into different ‘body plans’ to do other functions by design?
Tracheal cells
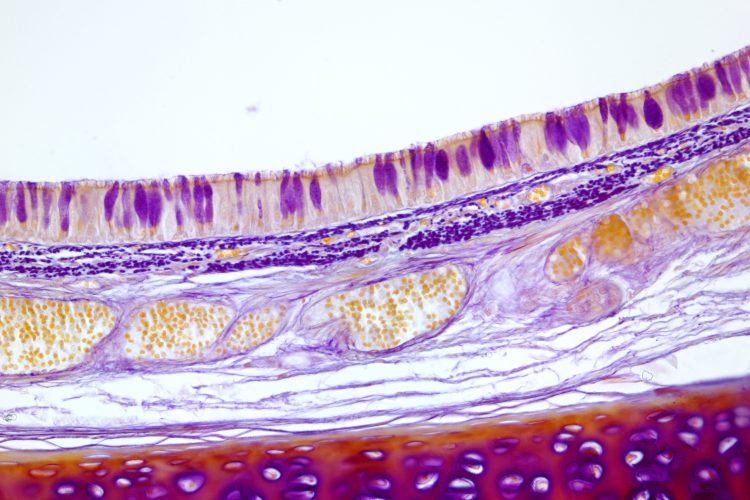
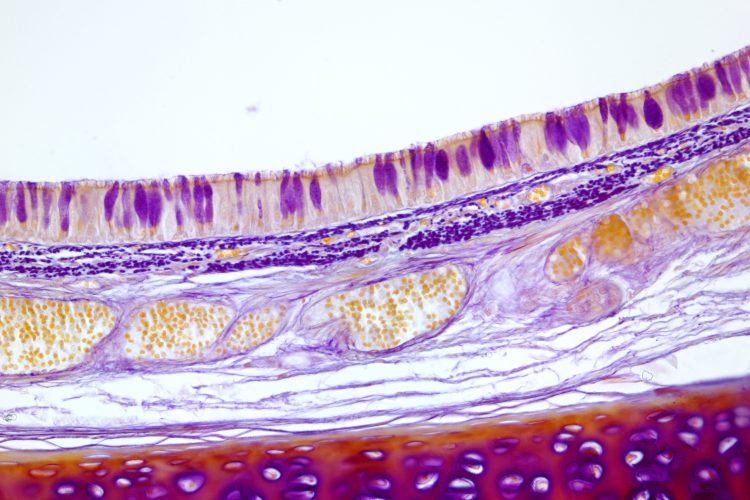
The scientists used tracheal cells to investigate how the human cells can create new structures and tasks. It was found that the cells both created new multicellular shapes and moved in different ways over a surface of human neurons grown in a lab dish, which encouraged new growth to fill in the gaps caused by scratching the layer of cells. Presently, it is unknown how anthrobots encourage the growth of neurons, although the researchers confirmed that neurons grew under the area covered by a cluster of anthrobots, termed a “superbot.”
Dr Levin explained: “It is fascinating and completely unexpected that normal patient tracheal cells, without modifying their DNA, can move on their own and encourage neuron growth across a region of damage.” He continued: “We’re now looking at how the healing mechanism works, and asking what else these constructs can do.”
Using human cells is advantageous as bots could be built from a patient’s own cells to perform therapeutic work without initiating an immune response or needing immunosuppressants, drugs prescribed to prevent rejection of transplanted tissues and organs which are also used in the treatment of autoimmune disorders.1
The bots last a week before breaking down so can be reabsorbed into the body easily. Furthermore, anthrobots can only survive in specific laboratory conditions when outside of the body, meaning there is no risk of exposure or unintended spread outside the lab. They do not reproduce or have genetic edits, additions, or deletions, so there is no risk of their evolving beyond existing safeguards.
Anthrobots
Anthrobots begin as a single cell from an adult donor. The cells are derived from the surface of the trachea and are covered with cilia which push out particles in the air passages of the lung. Previous studies by other researchers have demonstrated that when the cells are grown in the lab, they spontaneously form tiny multicellular spheres named organoids.
In the new study, the cilia were encouraged to face outward on the organoids by the scientists developing certain growth conditions. They began to move around within a few days, driven by the cilia. The first significant feature seen of the biorobotics platform was the different shapes and types of movement.
Dr Simon Garnier from the New Jersey Institute of Technology collaborated with the team to characterise the various types of anthrobots that were produced. In terms of shape, the bots ranged in size from 30 to 500 micrometres, filling a niche between nanotechnology and larger engineered devices. Also, some were spherical and fully covered in cilia and some were irregular with patchy coverage of cilia or covered with cilia only on one side.
In terms of movement, the bots travelled in straight lines, tight circles, a combination of both, or just wiggled in the same place. Typically, the spherical, fully covered in cilia bots wiggled, whilst ones with an uneven distribution of cilia moved forward for longer stretches in either straight or curved paths. These survived for between 45 to 60 days in laboratory conditions before biodegrading.
“It’s fully scalable—we can produce swarms of these bots in parallel, which is a good start for developing a therapeutic tool.”
Gumuskaya, who created the anthrobots, detailed: “Unlike xenobots, they don’t require tweezers or scalpels to give them shape, and we can use adult cells – even cells from elderly patients – instead of embryonic cells. It’s fully scalable—we can produce swarms of these bots in parallel, which is a good start for developing a therapeutic tool.”
Neuron layer
Levin and Gumuskaya aim to create anthrobots with therapeutic applications. Therefore, they made a model which was a two-dimensional (2D) layer of human neurons to observe how the bots heal wounds. They scratched the layer with a thin metal rod to form an open wound devoid of cells.
To ensure the wound would be exposed to a dense concentration of bots, they created superbots which were mainly circlers and wigglers, so would not stray far. The unmodified anthrobots triggered substantial regrowth, forming a bridge of neurons as thick as the rest of the healthy cells on the plate.
Further development of the bots may lead to other applications, including clearing plaque buildup in the arteries of atherosclerosis patients. In theory, they could help heal tissues, whilst laying down pro-regenerative drugs.
This study was published in Advanced Science.
Reference
1 Armstrong SC, Cozza KL, DiMartini AF, Fireman M. Immunosuppressants. Psychosomatics. 2004 July [2023 December 18]; 45(4):354-60. Available from: https://doi.org/10.1176/appi.psy.45.4.354
Related topics
Drug Delivery, Genome Editing, Neurons, Organoids
Related conditions
Atherosclerosis
Related organisations
Harvard University’s Wyss Institute, New Jersey Institute of Technology, Tufts University, University of Vermont