New models for intranasal drug delivery
Posted: 6 August 2021 | Dr Jon Lenn (MedPharm), Dr Jon Volmer (MedPharm) | No comments yet
In this article, Dr Jon Volmer and Dr Jon Lenn discuss a new approach to formulation models to test drug delivery based on reconstituted nasal epithelium.


The nasal cavity has enormous potential as a site for topical and systemic drug delivery. Delivery of intranasal drugs is relatively easy and painless, can lead to a rapid onset of pharmaceutical action and can be easily performed in emergency situations. In addition, drugs delivered intranasally can directly target the central nervous system (CNS).
However, the development of these new intranasal formulations depends on appropriate modelling of the nasal epithelium. Here, we assess reconstituted nasal epithelium (RNE) models – one of the latest for de-risking and expediting drugs formulated for intranasal delivery. The model, generated from human nasal epithelial cells, has a huge variety of potential applications, including in the modelling of respiratory diseases, such as COVID-19.
Assessing historical models
One of the most successful in vitro models for screening formulations for nasal delivery involves excised animal nasal mucosa (eg, sheep) mounted on a Franz cell. To determine formulation performance using this model, experimenters typically apply formulations to the apical side of the tissue and then sample receptor solution from the basolateral side.
This model is widely used and successful, with applications in the development of several drug products. However, it has several limitations, all of which are related to how it represents the active components of the mucosal barrier.
The nasal epithelium is characterised by tight junctions, a complex mucous layer, metabolism and active transport, all effected by the living epithelial cells. These epithelial cells form a complex layer that covers broad, rigid, highly vascularised structures called turbinates. Turbinates moisten, filter and warm air on its way to the lungs, which means they capture droplets or particles of active pharmaceutical ingredient (API) contained in sprays and powders. The highly vascularised nature of these structures allows for rapid delivery of API to the bloodstream.
Drug delivery is complicated in the nasal cavity by the tight junctions, protective mucus and ciliated cells. If a drug becomes trapped in mucus, it is then transported via ciliary action to the pharynx for removal. As a result, any drug needs to act or be absorbed rapidly before it is removed from the nose by ciliary action – or metabolised by the epithelial cells and components of the mucus.
…the development of these new intranasal formulations depends on appropriate modelling of the nasal epithelium”
The olfactory bulb, located above and behind the turbinates, is a section of specialised tissue that acts as the olfactory sensory organ. Due to its location and underlying structure, this patch of epithelium allows for direct and rapid access to the CNS, bypassing the blood-brain-barrier entirely.
Again, protective mucus and tight junctions are issues for drug absorption in the olfactory bulb, but it is hard to model drug interactions with this structure and the nasal cavity with an animal excised mucosa model. This is because the cilia, tight junctions, metabolic activity and mechanisms for mucus production are not present.
Developing an improved model
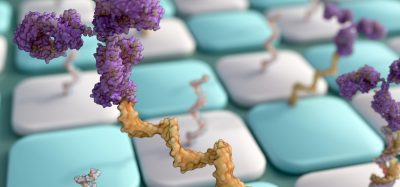
Today, new models are being developed that build and improve upon the excised nasal animal mucosa model. These include an RNE model, which uses primary human nasal epithelial cells harvested from the mucosa at the turbinates and regrown on permeable inserts.


At this point, the media is changed and the apical surface kept dry to promote full differentiation, which occurs over the span of three or four additional weeks. Over this time, the epithelial cells adopt a pseudostratified columnar compound epithelial layer. Upon full differentiation, the cells produce mucus, display ciliary activity and form tight junctions. This architecture typically persists for approximately four weeks and the integrity of the barrier can be monitored throughout the process by transepithelial electrical resistance (TEER).
Translating into practice
RNE cultures resemble more closely the nasal mucosal barrier than previous in vitro models. They also allow for additional analyses that are not possible using ex vivo tissue. These can include assessing the irritation potential of a formulation or drug or studying how mucus and ciliary action can impact the permeation of a formulation.
The RNE model can also be adapted for bronchial epithelium, allowing for the testing of new formulation types, such as those for the treatment of asthma, chronic obstructive pulmonary disease (COPD) and cystic fibrosis (CF). In the case of CF (and other genetic diseases), epithelial constructs can be grown from cells collected from the affected patient population during routine medical care.
In addition, the model can be extended to include nasal infection. The COVID-19 pandemic has highlighted the role of the nasal epithelium in infection and viral propagation and subsequently the importance of good models of infection. Modelling infection in RNE bypasses many well-known shortcomings associated with cell lines (such as the classical HBE4 and A549 cell lines).
…new models are being developed that build and improve upon the excised nasal animal mucosa model”
The shortcomings associated with cell lines have special importance in viral infection models, as the conditions in the host cell (such as protease and receptor expression) can generate artificial selection during propagation and infection. This selection can cast doubt on results from such work. Although the use of RNE does not eliminate this effect, it can reduce it.
Finally, the applications of RNE and other airway epithelial models can be further expanded using co-culture systems. Co-culture with inflammatory cells can be used to compare the performance of anti-inflammatory and antibiotic drugs. Reconstructed airway tissue can be co-cultured with airway smooth muscle to compare drugs for treating airway hyperresponsiveness in asthma. Due to the long-term viability of RNE constructs, tissue recovery from irritants – such as smoke, diesel exhaust particles and other environmental contaminants – can also be compared and monitored.
A final thought
The creation of new models for screening is critical to advancing drug development and delivery, especially of intranasal formulations. This exciting new RNE model for intranasal delivery improves upon traditional in vitro models and has the potential to help pharmaceutical companies de-risk and expedite their development programmes.
About the authors




Related topics
Assays, Cell Cultures, Cell-based assays, Central Nervous System (CNS), Drug Delivery, Drug Development, In Vitro
Related conditions
Asthma, Chronic obstructive pulmonary disease (COPD), Covid-19, Cystic fibrosis (CF)