Transporting antibodies across the blood–brain barrier to treat Alzheimer’s disease
Posted: 13 March 2023 | Ria Kakkad (Drug Target Review) | No comments yet
Researchers have found a way to ensure that new Alzheimer’s medications are delivered to the right place in the body and at the right timepoint in disease progression, so that they have the best effect.


In a study published recently in the Journal of Nanobiotechnology, researchers led by Tokyo Medical and Dental University (TMDU), Japan, have revealed that a novel delivery system delivers treatment to where it is needed most in a mouse model of Alzheimer’s disease.
Alzheimer’s is a common neurodegenerative disease that causes dementia. It is characterised by the accumulation of a protein called amyloid β (Aβ) in the brain, and several different toxic forms of Aβ have been identified that impair brain function, notably Aβ oligomers (AβOs).
“Multiple clinical trials have attempted to use an anti-Aβ antibody to treat Alzheimer’s, but the results have been unsatisfactory,” said lead author of the study Akiko Amano. “One potential explanation for this is that the blood–brain barrier (BBB) prevents most full-length antibodies from entering the brain.”
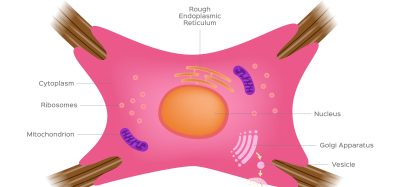
To address this challenge, the researchers previously developed glucosylated (sugar-linked) polymeric nanomicelles (PMs), which are tiny, hollow balls that could successfully cross the BBB via transcytosis in mouse brain capillary endothelial cells; this process was mediated by glucose-transporter-1 and induced by an increase in blood glucose levels after the mice experienced fasting conditions. In this study, the team filled PMs with fragments of an anti-AβO antibody, injected them into a mouse model of Alzheimer’s, and assessed the effects on the brain and on behaviour.
“The results were very clear,” explained senior author Nobuo Sanjo. “Administration of anti-AβO antibody fragments through PMs significantly reduced the amounts of various toxic Aβ species. In addition, the Aβ plaques that did form were smaller and less dense than those seen in untreated mice.”
Next, the researchers analysed the behaviour of the mice and found that the mice treated with the antibody fragment-filled PMs had better learning and spatial memory than untreated mice. “Our findings suggest that delivering sufficient levels of antibodies to the brain using PMs can reduce toxic Aβ species and slow Alzheimer’s progression in mice,” said Amano.
Given that the failure of anti-Aβ antibodies to improve cognitive function in human clinical trials was likely because of an insufficient supply of the antibodies in the brain, PM-encapsulated antibody fragments could represent an effective way to prevent Alzheimer’s progression. In addition, new candidates for Alzheimer’s treatment that degrade toxic Aβs and reduce their toxic effects could also be delivered to the brain using the same PM-based system.
Related topics
Antibodies, Disease Research, Drug Delivery, Neurosciences
Related conditions
Alzheimer’s disease
Related organisations
Tokyo Medical and Dental University (TMDU)
Related people
Akiko Amano, Nobuo Sanjo