Study identifies microbe-gut signalling as potential new treatment for IBD
Posted: 11 April 2023 | Ria Kakkad (Drug Target Review) | No comments yet
New research from Cincinnati Children’s Hospital Medical Center suggests blocking IL-22 and IL-1R could offer a promising IBD treatment.
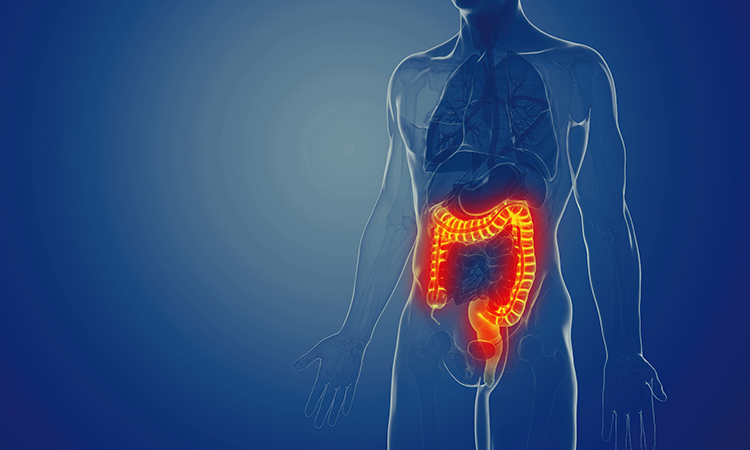
A recent study conducted by researchers at Cincinnati Children’s Hospital Medical Center, US, sheds new light on the signalling pathways between immune cells and gut epithelial cells in the presence of harmful intestinal inflammation. The study, published in the Journal of Experimental Medicine, could lead to a potential new treatment for inflammatory bowel disease (IBD), such as Crohn’s disease and ulcerative colitis.
IBD is a chronic inflammatory disorder that affects the digestive tract, and it has become a significant health problem globally. While past treatments for IBD focused on inhibiting IL-1β activity, these treatments had mixed results. However, the recent study reveals a new pathway that could be targeted for more effective treatment.
The research team conducted numerous experiments to learn about how immune cells located in the lining of the intestine detect and respond to microbes and relay important signals to gut epithelial cells. When the signalling networks between immune cells and epithelial cells function correctly, the immune system can live in harmony with friendly bacteria residing in the gut. But when the signalling is disrupted, the immune system can either fail to react or overreact, leading to IBD.
The study found that microbes are detected by cells of the immune system located in the intestines. These immune cells deliver signals to induce a protein called IL-1, which increases levels of another protein called IL-22. In turn, IL-22 begins acting in concert with IL-1 to activate the IL-1 receptor (IL-1R) expressed on intestinal epithelial cells. Activation of IL-1R induces ROS gene activity, in addition to other genes that recruit inflammatory cells to the tissue. This chain reaction drives an excessive inflammatory response that can damage the intestine, leading to IBD.
“The pathogenic role that IL-22 appears to play in inflammatory responses – due to its synergy with IL-1R signalling – had not been made clear previously,” said Dr Chandrashekhar Pasare. “We believe this may help explain why past treatments for IBD that focused only on inhibiting IL-1β activity had mixed results. We believe that a combined blockade of both IL-22 and IL-1R could serve as a more promising treatment for IBD.”
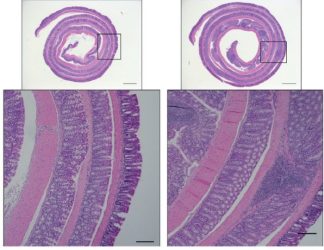
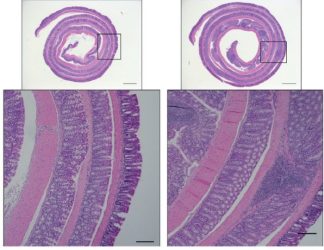
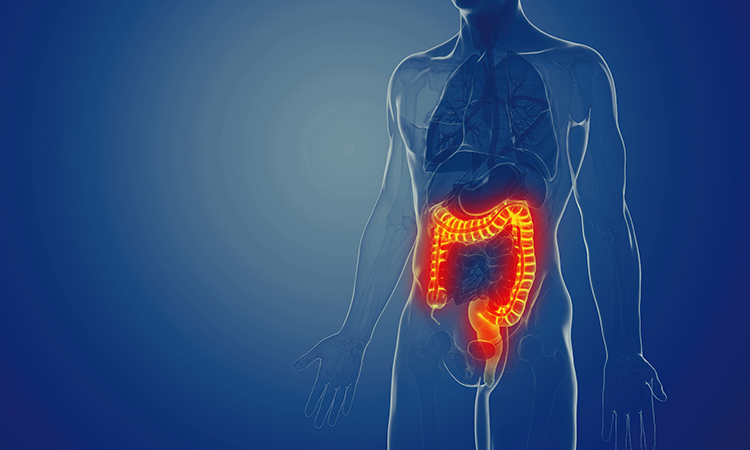
Control mice show the ability to clear away an experimental infection (images in the left column). But mice with impaired antimicrobial programs show increased intestine damage and inflammation (images in the right column), according to a study published in the Journal of Experimental Medicine [Credits: Cincinnati Children’s].
The researchers suggest that monoclonal antibodies that can inhibit IL-22 or IL-1R, which have been evaluated in clinical trials for various auto-immune conditions, could be safely used in combination therapy or that new treatments targeting the two pathways could be developed. The study’s findings provide hope for new, effective treatments for IBD that could improve the quality of life for millions of people worldwide.
Related topics
Cell Therapy, Disease Research, Immunotherapy
Related conditions
Crohn’s disease, Inflammatory bowel disease (IBD)
Related organisations
Cincinnati Children's Hospital Medical Center
Related people
Dr Chandrashekhar Pasare