New insights about the development of hematopoietic stem cells
Posted: 21 December 2023 | Drug Target Review | No comments yet
Understanding the involvement of Nod1 in the development of blood stem cells could greatly improve blood disorder treatments.
Iowa State University researchers have new insights into how a microbial sensor that helps identify and fight bacterial infections also has a crucial part in the development of blood stem cells.
Led by Dr Raquel Espin Palazon, an Assistant Professor of Genetics, Development and Cell biology at Iowa State University, the team’s study builds on Palazon’s previous work showing that the inflammatory signals that initiate a body’s immune response have a completely different role in the earliest stages of life, as vascular systems and blood are forming in embryos.
Knowing that embryos activate the microbial sensor, a protein known as Nod1, to force vascular endothelial cells to become blood stem cells could help develop a method to produce blood stem cells in a lab from a patient’s own blood, Palazon said. She commented: “This would eliminate the challenging task of finding compatible bone marrow transplant donors and the complications that occur after receiving a transplant, improving the lives of many leukaemia, lymphoma and anaemia patients.”
Immune receptor
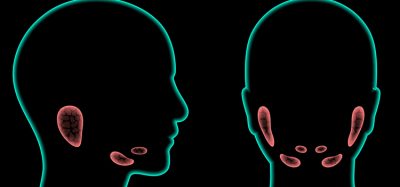
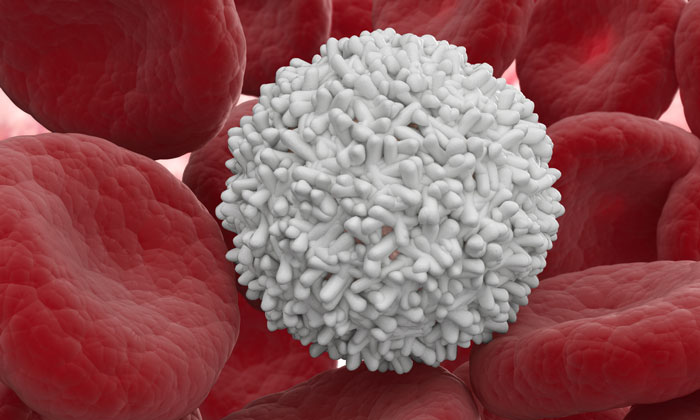
Stem cells repeatedly divide to self-renew and form new cells for specific tissues. Pluripotent stem cells in embryos can differentiate into any kind of cell required by the body but adult stem cells are limited to producing particular types. Blood stem cells, known as hematopoietic stem cells, make all of blood’s components and a lifetime supply of blood stem cells is created inside an embryo before birth.
“We didn’t know that this receptor was needed or that it was needed this early, before blood stem cells even form.”
Palazon’s team found the immune receptor that activates in an embryo before endothelial cells start becoming stem cells, priming them for the transition. “We know blood stem cells form from endothelial cells, but the factors that set up the cell to switch identity were enigmatic,” Palazon said. “We didn’t know that this receptor was needed or that it was needed this early, before blood stem cells even form.”
Nod1 was found through analysis of public databases of human embryos. They studied it using zebrafish, which share about 70 percent of their genome with humans, tracking blood stem cell creation carefully with Nod1 levels as its effects were inhibited or enhanced.
The team also worked with the Children’s Hospital of Philadelphia to confirm that Nod1 is involved in human blood development. Researchers there produced human induced pluripotent stem cells (hiPSCs), which are generated from mature samples but genetically reprogrammed to act like the stem cells found in embryos.
Although induced pluripotent stem cells can create most types of blood cells, they cannot produce functional blood stem cells. However, when researchers took away Nod1, blood production faltered, as it did with blood stem cells in zebrafish.
Advancing regenerative medicine
Understanding that Nod1 is a prerequisite for blood stem cells to develop is progress for scientists hoping to design a system for producing blood stem cells from human samples. This could provide a great new option for patients suffering from blood disorders. Patients could be treated with stem cells that originated in their own body, instead of needing a life-saving infusion of blood stem cells via a transplant of bone marrow, the spongy insides of bones that holds most of a body’s blood stem cells. This would avoid the risks of graft-versus-host disease, a common and potentially deadly reaction that happens when a patient’s immune system attacks the transplant. Palazon stated: “This would be a huge advancement for regenerative medicine.”
The team are continuing to study the interactions in which blood stem cells arise, including refining the timeline. Understanding when signals are expressed is key to developing the methods for making blood stem cells.
“I believe our investigations will pave the road to finally create therapeutic-grade blood stem cells to cure blood disorder patients,” Palazon concluded.
This study was published in Nature Communications.
Related topics
Cancer research, Research & Development, Stem Cells
Related conditions
anaemia, Cancer Research, Leukaemia, lymphoma
Related organisations
Children's Hospital of Philadelphia, Iowa State University
Related people
Dr Raquel Espin Palazon (Iowa State University)