New strategies to overcome CAR T-cell resistance in AML cells
Posted: 22 March 2024 | Drug Target Review | No comments yet
Pharmacological concomitant therapies or further genetic improvement of CAR T-cells can increase their effectiveness against TP53-mutant AML cells.
Researchers from the University of Zurich (UZH) have demonstrated that TP53-mutant acute myeloid leukaemia (AML) cells are significantly more resistant to CAR T-cell therapy compared to AML cells without the mutated gene.
AML, an aggressive form of blood cancer, is caused by mutations in many genes that are acquired during a person’s life. One of these genes is the tumour suppressor gene TP53, which normally helps to prevent the development of tumours. However, if patients have the mutated form, they face an extremely poor prognosis as their genes become resistant to conventional chemotherapeutic agents.
Therefore, intensive research is being conducted to find new therapeutic approaches, like CAR T-cells, which are already being used successfully for other cancers of the blood.
Dr Stephan Boettcher, chief of service at the University Hospital Zurich (USZ), explained: “The reason for the poorer effect of CAR T-cells with mutated TP53 is that these immune cells are exhausted more quickly and are therefore less active against the cancer cells.”
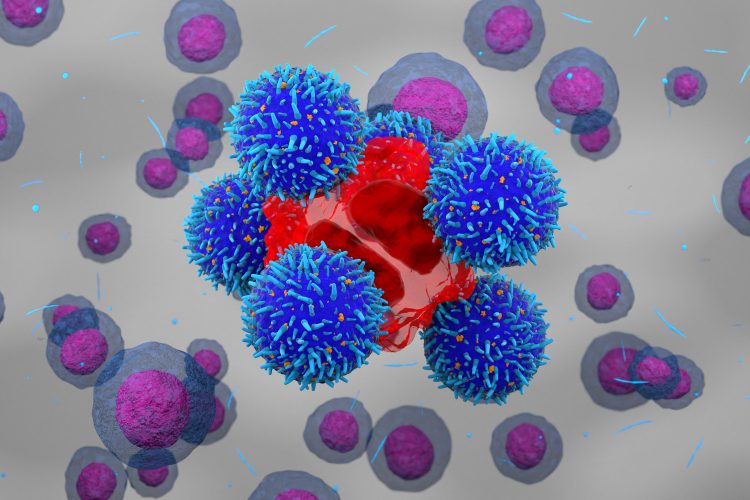
In CAR T-cell therapy, T-cells are extracted from a patient’s blood and are then genetically modified in the lab so that they form multiple new contact points (CARs) on their surface. When reintroduced into the patient, these CAR T-cells can recognise certain surface structures on the tumour cells, allowing them to destroy the cancer cells in a targeted manner. Currently, there are various CAR T-cell products being tested against AML in early clinical trials.
Led by Dr Boettcher and Dr Markus Manz, the team examined the mechanism underlying the resistance of mutated AML cells to CAR T-cell immunotherapy. They also discovered how the endurance of CAR T-cells can be increased, and how a weak point of TP53-mutant AML cells can be exploited to overcome this resistance.
They were able to greatly increase the effectiveness of CAR T-cells against TP53-mutant AML cells through additional pharmacological concomitant therapies or further genetic improvement of the CAR T-cells, to the point where there was no longer any therapeutic difference compared to non-mutated AML cells.
Dr Manz concluded: “This proof-of-principle study shows that concurrent pharmacological therapies and genetically engineered CAR T-cells are promising strategies to develop more effective and tolerable immunotherapies for patients with TP53-mutant AML.”
This study was published in EMBO Molecular Medicine.
Related topics
Cancer research, Cell Therapy, Chimeric Antigen Receptors (CARs), Drug Development, Immuno-oncology, Immunotherapy
Related conditions
acute myeloid leukaemia (AML)
Related organisations
University Hospital Zurich (USZ), University of Zurich (UZH)
Related people
Dr Markus Manz (USZ), Dr Stephan Boettcher (USZ)