Stanford grows vascularised mini-organs
Posted: 16 June 2025 | Drug Target Review | No comments yet
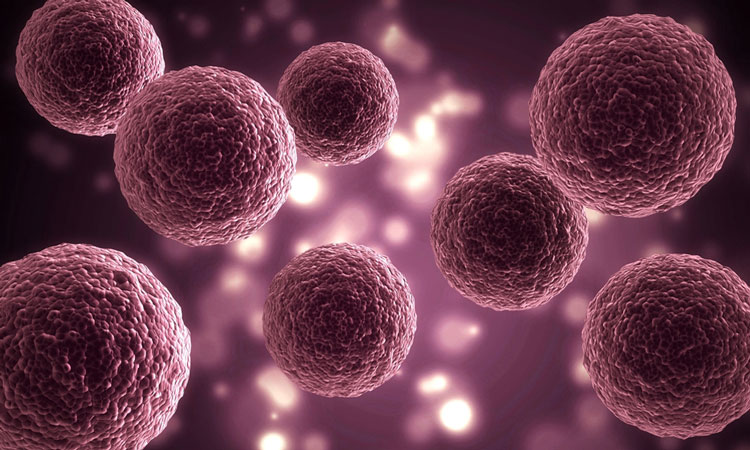
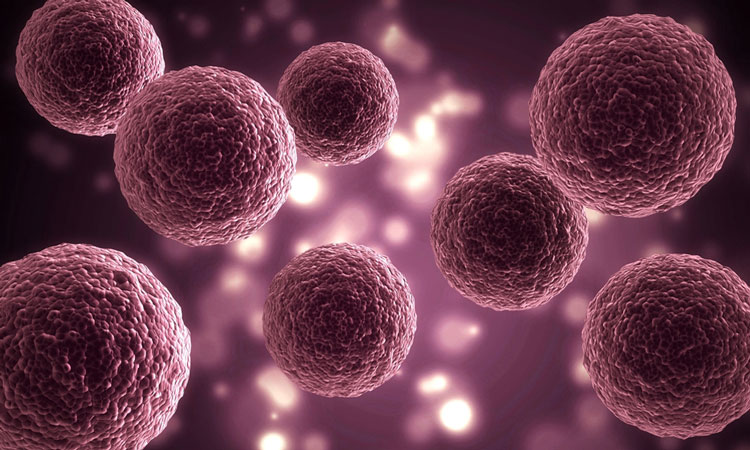
Stanford scientists have successfully grown heart and liver organoids that include functioning blood vessels. This breakthrough overcomes a major size and maturity barrier, which could advance disease modelling and regenerative therapies in the future.
For over ten years, scientists have relied on miniature, lab-grown clusters of human cells that mimic real organs, called organoids, to study diseases and test therapies. These organoids have been used to model everything from neurodevelopmental disorders with brain organoids to SARS-CoV-2 infections in lung models. Some, like heart organoids, have even been sent to space to test the effects of microgravity.
But they have one major limitation: organoids can’t grow larger than about approximately 3 millimetres, the size of a sesame seed. Unlike organs in the human body, organoids lack blood vessels, which deliver oxygen and nutrients to cells. Without this vascular system, organoids die from the inside out as they grow.
“When you grow organoids to a certain size they start to die inside because they can’t get oxygen and nutrients to the centre,” said Dr Oscar Abilez, MD, a senior scientist in the Division of Paediatric Cardiac Surgery at Stanford Medicine.
Automation now plays a central role in discovery. From self-driving laboratories to real-time bioprocessing
This report explores how data-driven systems improve reproducibility, speed decisions and make scale achievable across research and development.
Inside the report:
- Advance discovery through miniaturised, high-throughput and animal-free systems
- Integrate AI, robotics and analytics to speed decision-making
- Streamline cell therapy and bioprocess QC for scale and compliance
- And more!
This report unlocks perspectives that show how automation is changing the scale and quality of discovery. The result is faster insight, stronger data and better science – access your free copy today
A breakthrough in vascularisation
That challenge may now be solved. In a study published in Science, Abilez and a team of Stanford Medicine researchers successfully grew heart and liver organoids complete with intricate networks of blood vessels. This innovation could allow organoids to grow larger and more closely mimic real human tissue.
“The ability to grow vascularised organoids overcomes a major bottleneck in the field,” said Abilez, a co-lead author of the study.
A step toward regenerative medicine
The new vascularised organoids could also be instrumental in regenerative therapies. In a related clinical study, the study’s senior author, Dr Joseph Wu, MD, and his team are already injecting lab-grown cardiomyocytes into patients with heart dysfunction.
The new vascularised organoids could also be instrumental in regenerative therapies
“But actual heart tissue contains more than cardiomyocytes,” Wu said. “There are endothelial cells that line blood vessels, smooth muscle cells that surround blood vessels, pericytes that connect blood vessels, fibroblasts and other cells.”
In the future, vascularised organoids made from a patient’s own stem cells might be surgically implanted to replace damaged tissue.
“The thought is that if organoids have a vascular system, they could connect with the host vasculature, and that’ll give them a better chance to survive,” Abilez explained.
Finding the right recipe
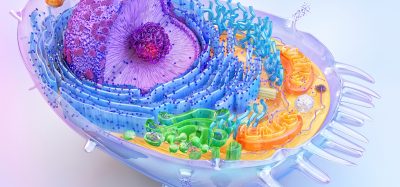
To create vascularised heart organoids, the team turned to a chemical approach rather than engineering or 3D printing. They reviewed existing protocols for producing three key heart cell types- cardiomyocytes, endothelial cells, and smooth muscle cells, then combined them into 34 different “recipes” using varying growth factors and dosages.
They also genetically modified the stem cells to glow in specific colours when they turned into each of the three cell types. One recipe stood out: condition 32.
“It was pretty obvious,” Abilez said. “We picked the one that gave us the most amount of those three fluorescent colors, which correspond to the most cardiomyocytes, endothelial cells and smooth muscles cells.”
Tiny organs with real blood vessels
Under 3D microscopy, the resulting doughnut-shaped heart organoids showed clearly defined structures: cardiomyocytes and smooth muscle cells on the inside, with an outer layer of endothelial cells forming branched, tubular blood vessels.
These blood vessels, which were about 10 to 100 microns in diameter, are similar in size to capillaries in the human heart.
Using single-cell RNA sequencing, researchers found that each organoid contained 15 to 17 different heart cell types. This is comparable to a six-week-old embryonic heart, which has 16, whilst an adult heart has 21.
“It had all these other cell types that are found in the heart,” Abilez said. “That was unexpected in a positive way.”
Opening the black box of development
The researchers believe their optimised recipe mimics early embryonic conditions, allowing the organoids to develop like a six-week-old fetal heart. This could make them powerful models for studying early human development.
“There’s this black box of development in early pregnancy when it’s not possible, ethically, to test drugs,” Abilez said.
As a test case, the researchers exposed vascularised cardiac organoids to fentanyl, a potent opioid. The organoids responded by producing more blood vessels.
“We don’t know how that might manifest in a newborn yet, but it’s a difference,” Abilez said.
Beyond the heart: liver and more
The same strategy was applied to liver organoids, resulting in robustly vascularised liver tissue. The researchers believe this method could be adapted for nearly any organ type.
“I’d love to be able to do this in all the different organoid types,” Abilez said. “After all, almost every organ in our body has a blood vessel system.”
Next, the team plans to allow the vascularised organoids to grow longer, tracking how large and mature they become. They also aim to fine-tune the recipes to include additional cells, such as immune and blood cells, to more accurately model adult human organs.
Related topics
Bioengineering, Cell Therapy, Disease Research, Drug Discovery, Drug Discovery Processes, Molecular Biology, Organoids, Regenerative Medicine, Stem Cells, Translational Science
Related conditions
Heart disease
Related organisations
Stanford Medicine