Protecting bones from cancer damage: targeting the UPR pathway
Posted: 29 September 2025 | Drug Target Review | No comments yet
New research highlights how cancer hijacks the unfolded protein response (UPR) in bone cells – potentially allowing for the development of therapies that target this pathway to prevent fractures.
Before a chain of amino acids can become an active protein, it must be processed and folded into the correct shape – this largely takes place in the endoplasmic reticulum (ER) of cells. When protein homeostasis is disrupted, the ER can become overwhelmed. To manage this, a safety mechanism called the unfolded protein response (UPR) activates, slowing protein synthesis to give the ER time to recover. If this temporary slowdown is insufficient – the UPR triggers cell death.
In many cancerous cells, however, the UPR is altered to prevent cell death, allowing malignant cells to survive in low-oxygen and low-nutrient tumour environments. This makes the UPR pathway a promising target for new cancer therapies.
How cancer hijacks bone health
Professor Sarah A. Holstein and Dr Molly E. Muehlebach from the University of Nebraska Medical Center have examined how the UPR relates to cancer-induced bone damage. Their review, published in Bone Research, analyses how the UPR is involved in bone cell differentiation and how cancerous infiltration of bone hijacks this system to weaken the skeleton.
This occurs in primary bone cancers like osteosarcoma and Ewing sarcoma, in blood cancers such as multiple myeloma and in solid tumours that metastasise to bone, including breast and prostate cancers.
“Disruption of the remodelling cycle can result in bone loss or increased bone density. However, in both cases, the bone is brittle and can easily fracture,” said Professor Holstein. “As a result, skeletal structure and integrity is compromised, significantly contributing to disease morbidity and negatively impacting overall patient survival in cancer-induced bone disease.”
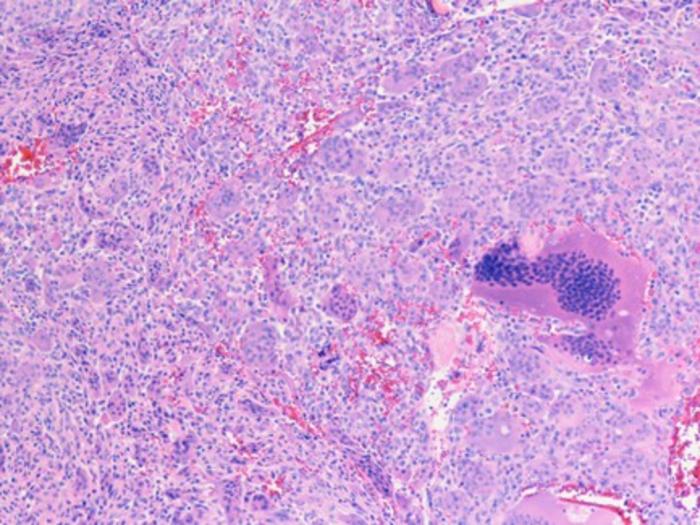
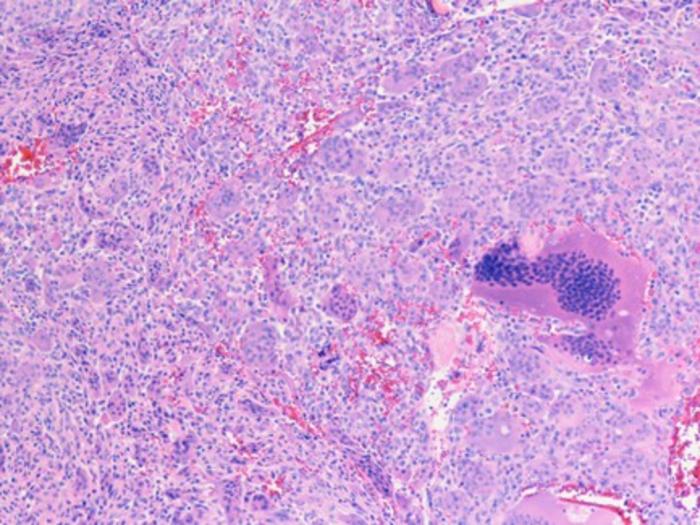
Drugs that interrupt the death of healthy bone cells and induce the death of cancerous cells located in bones can prevent or reduced cancer associated bone weakness and improve treatment outcomes for patients. Credit: “Giant cell tumor of bone, tibia” by cnicholsonpath Image Source Link: https://openverse.org/image/721cc46f-5def-41cc-a970-739c99d10a34
Mapping the UPR pathways in bone
The study highlights the three primary UPR pathways – EIF2AK3, ERN1and ATF6 – and their downstream signalling cascades. Professor Holstein and Dr Muehlebach detail how UPR-associated proteins influence the differentiation of osteoblasts (bone-building) and osteoclasts (bone-resorbing) cells. Maintaining the balance between these two cell types is vital for healthy bones.
When cancer cells invade bone tissue, they disrupt the UPR, leading to dysfunction of osteoclasts, osteoblasts, or. This results in bones that are either weak from low density or brittle from excessive mineralisation. These complications are named skeletal related events (SREs).
Emerging therapies targeting UPR
There are several new, emerging drug classes that aim to reduce SREs by targeting specific UPR pathways:
- Inhibiting EIF2AK3: GSK2606414
- Inhibiting ERN1: sunitinib malate, toyocamycin
- Inhibiting ER-associated protein degradation: VCP inhibitors such as CB-5083
- Enhancing chaperone proteins: sodium phenylbutyrate
Other drugs with high bone tissue affinity may induce UPR-mediated apoptosis in malignant cells by disrupting protein processing:
- Disrupting isoprenoid synthesis: bisphosphonates zoledronic acid (ZA) and RAM2061
- Disrupting unfolded protein degradation: oprozomib
These therapies are at various stages of in vitro, animal or early human trials and show promise in alleviating SREs and killing bone-localised tumours. Researchers warn that much work remains to ensure these drugs target cancerous cells without harming healthy bone or other tissues.
“Ultimately, the success of UPR modulators in treating cancer-related bone disease will depend on developing agents that specifically target bone and tumour cells while minimizing effects on healthy tissue,” said Professor Holstein.
Related topics
Cancer research, Drug Discovery, Drug Discovery Processes, Drug Targets, Oncology, Protein, Therapeutics, Translational Science
Related conditions
Cancer
Related organisations
the University of Nebraska Medical Center



