Injecting VIP into the eye improves corneal transplant survival
Posted: 13 August 2018 | Drug Target Review | No comments yet
Results using mouse models suggest that vasoactive intestinal peptide may provide a new method of improving the outcomes of corneal transplant surgery…
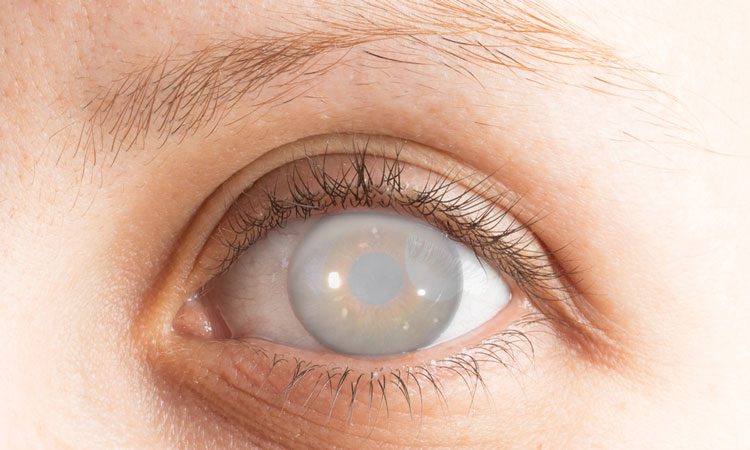
Injecting neuropeptide vasoactive intestinal peptide (VIP) directly into the eye of mice enhanced corneal graft survival.
A team of researchers from Harvard Medical School found that VIP also produced other benefits such as accelerating the endothelial wound closure, protecting the corneal endothelial cells (CEnCs) and improving the clarity of the corneal graft.
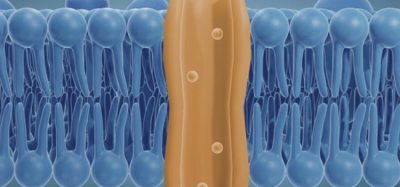
VIP is a 28 amino acid peptide and is recognised as an immunoregulatory and protective factor in various organ systems. Found in the aqueous humour of the eye, and possibly secreted by CEnCs, VIP is known to help preserve the integrity of CEnCs.
Biomarkers aren’t just supporting drug discovery – they’re driving it
FREE market report
From smarter trials to faster insights, this report unpacks the science, strategy and real-world impact behind the next generation of precision therapies.
What you’ll unlock:
- How biomarkers are guiding dose selection and early efficacy decisions in complex trials
- Why multi-omics, liquid biopsy and digital tools are redefining the discovery process
- What makes lab data regulatory-ready and why alignment matters from day one
Explore how biomarkers are shaping early drug development
Access the full report – it’s free!
“The successful outcome of corneal transplantation mainly relies on the density and function of CEnCs, which keep the graft transparent. To improve the outcomes of corneal transplantation, various strategies have been employed to prevent immune-mediated graft rejection or enhance survival and function of CEnCs. However, an effective method has remained elusive so far,” explained Dr Ahmad Kheirkhah, who completed the research while he was at the Massachusetts Eye and Ear, Department of Ophthalmology, Harvard Medical School.
The team investigated the effect of VIP on corneal tissue in cell culture, and in vivo, where living mice received corneal transplants. In cell cultures of human corneal endothelial cells, VIP accelerated wound healing, and when the corneal cells were exposed to compounds known to cause apoptosis, such as interferon-y or tumour necrosis factor-a, VIP displayed a dose-dependent protective effect.
In VIP treated mouse models, grafts were more transparent than in non-VIP treated mice. After eight weeks, 85 percent of grafts that had the VIP treatment survived, compared with 0 percent of those not treated. Researchers also found that corneal endothelial cell density was greater in treated corneas, compared with untreated corneas.
“Millions of patients around the world are blind due to corneal opacity, and they are in dire need of corneal transplantation. Unfortunately, there is a significant shortage of donor corneas across the world. On the other hand, many donated corneas cannot be used for transplantation due to inadequate endothelial cells. Moreover, corneal transplants can deteriorate over time due to continuous loss of CEnCs,” noted Professor of Ophthalmology at the Massachusetts Eye and Ear, Harvard Medical School, Dr Reza Dana.
“If confirmed in further clinical studies, we believe that the use of VIP will increase the number of donated corneas suitable for transplantation and improve the outcomes of corneal transplantation.”
The study was published in the American Journal of Pathology.
Related topics
Disease Research, Drug Development, In Vivo, Research & Development
Related conditions
corneal opacity
Related organisations
Harvard Medical School
Related people
Dr Ahmad Kheirkhah, Dr Reza Dana