Rod-shaped microparticles could improve immune system response to COVID-19
Posted: 11 June 2020 | Victoria Rees (Drug Target Review) | No comments yet
Researchers have suggested that neutrophils, which contribute to the development of ARDS in COVID-19 patients, could be diverted from the lungs by rod-shaped particles in a new form of treatment.
According to new research, a specific white blood cell may be central to the immune system overreaction that is the most common cause of death for COVID-19 patients and particular elongated, rod-shaped particles could be used to take these out of circulation.
The study was conducted by University of Michigan (U-M), US, researchers. The team highlight that acute respiratory distress syndrome (ARDS) could be prevented by drawing certain immune cells out of the lungs of COVID-19 patients.
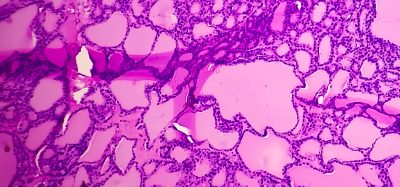
ARDS is a manifestation of a condition known as cytokine storm, in which the immune system overexpresses itself and begins attacking the body’s own organs. In ARDS, white blood cells break down lung tissue and cause fluid to build up in the lungs. A major driver of this event is a type of white blood cell called a neutrophil, which makes up 60 to 70 percent of intruder-eating ‘phagocyte’ cells in humans.
“Their main job is to make sure your boundaries aren’t breached,” said lead researcher Lola Eniola-Adefeso, professor of biomedical engineering and professor of macromolecular science and engineering.
The researchers say that as neutrophils are not specialised, this enables them to respond to many threats. However, this lack of specialisation can mean the cells continue their role even when not required to.
“As long as there’s cues, neutrophils keep acting. In some instances, the feedback loop is broken and that turns what is meant to be a good response into a bad response,” Eniola-Adefeso said.
One of their actions is to emit signalling molecules called cytokines that tell cells to break down barriers and let blood and fluid into a problem site. When that response becomes detrimental, the neutrophils need to be stopped so that other cells can step in and repair the damage.
Previously, Eniola-Adefeso’s group showed that plastic microparticles injected into the blood of mice could distract neutrophils, diverting them away from areas of severe inflammation in their lungs. The neutrophils would grab the particle and move to the liver to dispose of it. Microplastics used in this way eased ARDS in mice.
However, any type of phagocyte might engulf a sphere, which means a sphere-based therapy is likely to affect other parts of the immune response. Instead, rod-shaped particles can be used to exclusively target neurtophils, which the researchers demonstrated have a preference for wrapping around elongated shapes.
The team found that when they offered rods to different phagocytes, 80 percent of the neutrophils ate them, whereas only five to 10 percent of other phagocytes did. The comparisons included macrophages, another cell that eats intruders and dendritic cells, which capture intruders and then show the other immune cells what to look for.
The team is currently exploring whether neutrophil-distracting particles can be made from medications rather than plastic. Eniola-Adefeso is now working with the U-M Office of Technology Transfer to advance her delivery system toward clinical trials, in hopes that it may prove useful in the fight against COVID-19.
U-M has applied for patent protection and has launched a start-up company, Asalyxa.
The study was published in Science Advances.
Related topics
Drug Discovery, Drug Targets, Research & Development, Target Molecule, Target Validation, Targets
Related conditions
Acute Respiratory Distress Syndrome (ARDS), Coronavirus, Covid-19
Related organisations
Michigan University
Related people
Lola Eniola-Adefeso