Promising new avenue to tackle obesity-related diabetes
Posted: 2 July 2021 | Mandy Parrett (Drug Target Review) | No comments yet
New findings from collaborative research in the United States have identified a promising new treatment avenue for type 2 diabetes patients centring on the activity of the amino acid, GABA.
With type 2 diabetes now 24 times more prevalent than type 1, scientists are keen to tackle the debilitating disease at a more fundamental level. The discovery of insulin transformed the lives of individuals whose bodies are unable to produce their own insulin, yet its use for type 2 diabetes patients merely aims to manage blood glucose levels.
Believing that a different tack was needed to address the root cause, a team of scientists led by Benjamin Renquist, an associate professor in the University of Arizona College of Agriculture and Life Sciences and BIO5 Institute member, has discovered that an amino acid GABA may hold the key to new treatment options.
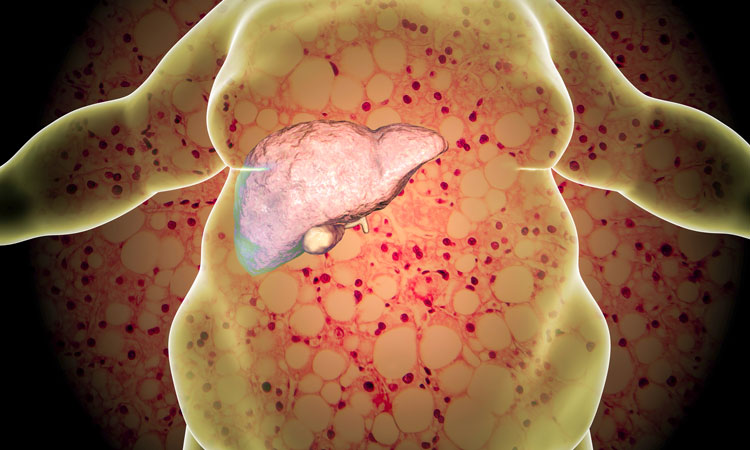
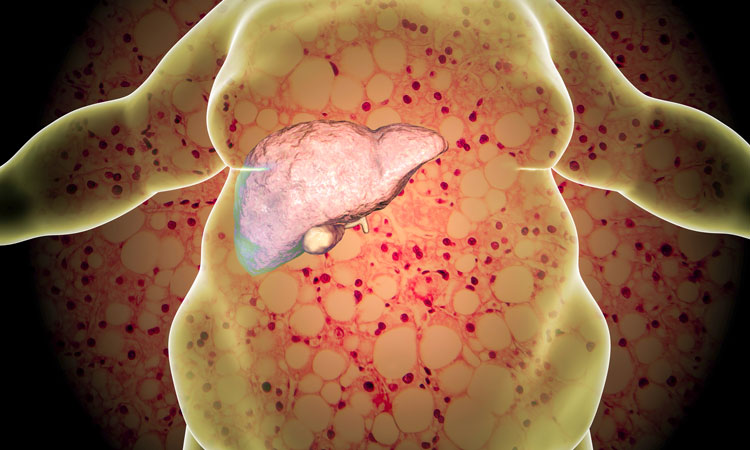
Renquist, whose research lab aims to address obesity-related diseases in general, has spent the last nine years working to better understand the correlation between obesity, fatty liver disease and diabetes, particularly how the liver affects insulin sensitivity.
“Obesity is known to be a cause of Type 2 diabetes and, for a long time, we have known that the amount of fat in the liver increases with obesity,” Renquist said. “As fat increases in the liver, the incidence of diabetes increases.”
However, the mechanism by which fat in the liver works to make the body resistant to insulin was unknown. Renquist, along with researchers from Washington University in St. Louis, the University of Pennsylvania and Northwestern University, focused on neurotransmitters in animal models of the disease, to understand the brain’s communication with the liver and vice versa.
In two papers outlining their findings, Renquist explained, “We found that fat in the liver increased the release of the inhibitory neurotransmitter Gamma-aminobutyric acid, or GABA,”
“We then identified the pathway by which GABA synthesis was occurring and the key enzyme that is responsible for liver GABA production – GABA transaminase.”
A naturally occurring amino acid, GABA is the primary inhibitory neurotransmitter in the central nervous system, meaning it decreases nerve activity.
Nerves are a conduit for communication between the brain and the rest of the body. That communication is not only from the brain to other tissues, but also from tissues back to the brain, Renquist explained.
“When the liver produces GABA, it decreases activity of those nerves that run from the liver to the brain. Thus, fatty liver, by producing GABA, is decreasing firing activity to the brain,” Renquist said. “That decrease in firing is sensed by the central nervous system, which changes outgoing signals that affect glucose homeostasis.”
To determine if increased liver GABA synthesis was causing insulin resistance, graduate students in Renquist’s lab, Caroline Geisler and Susma Ghimire, pharmacologically inhibited liver GABA transaminase in animal models of Type 2 diabetes.
“Inhibition of excess liver GABA production restored insulin sensitivity within days,” said Geisler, now a postdoctoral researcher at the University of Pennsylvania and lead author on the papers. “Longer term inhibition of GABA-transaminase resulted in decreased food intake and weight loss.”
To ensure the findings would translate to humans, Kendra Miller, a research technician in Renquist’s lab, identified variations in the genome near GABA transaminase that were associated with type 2 diabetes. Collaborating with investigators at Washington University, the researchers showed that in people with insulin resistance, the liver more highly expressed genes involved in GABA production and release.
The findings are the foundation of an Arizona Biomedical Research Commission-funded clinical trial currently underway at Washington University School of Medicine in St. Louis with collaborator Samuel Klein, co-author on the study and a Washington University professor of medicine and nutritional science. The trial will investigate the use of a commercially available Food and Drug Administration-approved inhibitor of GABA transaminase to improve insulin sensitivity in people who are obese.
“A novel pharmacological target is just the first step in application; we are years away from anything reaching the neighbourhood pharmacy,” Renquist said. “The magnitude of the obesity crisis makes these promising findings an important first step that we hope will eventually impact the health of our family, friends and community.”
The papers were published in Cell Reports.
Related topics
Amino Acids, Analysis, Clinical Trials, Disease Research, Drug Targets, Enzymes
Related conditions
Type-2 diabetes
Related organisations
Arizona Biomedical Research Commission, Northwestern University, Pennsylvania University, University of Arizona (UArizona), Washington University
Related people
Benjamin Renquist