Automated red blood cell exchange: bridging treatment gaps in sickle cell disease care
Posted: 5 June 2025 | Carly Newton (Senior Manager of Apheresis Clinical Marketing at Terumo Blood and Cell Technologies), Dr Aaron Haubner (Senior Manager of North America Medical Affairs and Market Access at Terumo Blood and Cell Technologies) | No comments yet
Despite the promise of gene therapies, automated red blood cell exchange (aRBCX) remains an underutilised therapy in the management of sickle cell disease (SCD). In this article, Dr Aaron Haubner and Carly Newton of Terumo Blood and Cell Technologies, highlight the urgent need for partnerships and equitable access to this life-saving treatment, offering immediate benefits by reducing complications and improving quality of life.
Despite recent advances in gene therapy for sickle cell disease (SCD), automated red blood cell exchange (aRBCX) remains a cornerstone therapy that plays a vital yet underutilised role in managing complications and enhancing quality of life for millions living with this devastating condition worldwide. Dr Aaron Haubner, Senior Manager of North America Medical Affairs and Market Access at Terumo Blood and Cell Technologies, reveals that while promising new treatments emerge, urgent partnerships are needed to ensure this essential blood therapy reaches the patients who need it most.
Introduction
In the US, sickle cell disease affects approximately 100,000 Americans, approximately 90 percent of whom are African American, with the remainder being Hispanic or Latino.1 About two-thirds of mothers of newborns with SCD live in US counties with high or very high levels of social vulnerability.1-3 These socio-economic determinants of health significantly impact outcomes, reflected in a dramatically reduced life expectancy of around 53 years – more than 20 years less than the general population.4
In the US, sickle cell disease affects approximately 100,000 Americans, approximately 90 percent of whom are African American, with the remainder being Hispanic or Latino.
The therapeutic landscape for SCD has evolved significantly in recent years. Currently, three FDA-approved disease-modifying drug therapies are available: hydroxyurea, crizanlizumab and L-glutamine, though each has limitations that affect patient compliance.5,6 The 2023 approval of two engineered stem cell-based therapies marked a significant advancement, though these options require careful consideration of potential adverse events and long-term safety,7 and access will remain a challenge for the foreseeable future.
Automation now plays a central role in discovery. From self-driving laboratories to real-time bioprocessing
This report explores how data-driven systems improve reproducibility, speed decisions and make scale achievable across research and development.
Inside the report:
- Advance discovery through miniaturised, high-throughput and animal-free systems
- Integrate AI, robotics and analytics to speed decision-making
- Streamline cell therapy and bioprocess QC for scale and compliance
- And more!
This report unlocks perspectives that show how automation is changing the scale and quality of discovery. The result is faster insight, stronger data and better science – access your free copy today
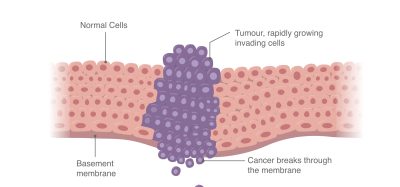
Transfusion-based blood therapies, the first disease-modifying therapies for SCD, remain a cornerstone of care. However, not all transfusion treatment options are the same. While simple transfusion requires no specialised equipment, it can lead to complications including iron overload (requiring chelation therapy) and alloantibody development that makes future blood matching increasingly difficult.9,12 Automated red blood cell exchange (aRBCX) addresses these challenges by maintaining fluid balance and minimising iron overload while systematically removing sickled cells and replacing them with healthy donor cells.14 This is achieved without adding adverse event or alloimmunisation risk compared to simple transfusion.8-14 Given its proven therapeutic benefits, aRBCX is recognised as the first-line treatment for acute stroke and stroke prevention in sickle cell disease, despite requiring specialised equipment and additional donor blood.14
In addition, the crucial role of aRBCx was recently highlighted via collaboration between international experts in disciplines affecting maternal health. Its unique advantages are particularly pertinent to high-risk pregnancies, where other disease-modifying therapies are often contraindicated or unproven.15 For this vulnerable population, aRBCX offers a proven, safe and effective treatment option, supported by expert consensus and clinical evidence.16,17 Beyond pregnancy care, it also serves as a valuable second-line therapy for managing acute chest syndrome and vaso-occlusive crises, making it an essential tool in comprehensive sickle cell care.17
Patient challenges and treatment potential
Despite the available therapeutic options, SCD remains significantly under-treated, with less than 30 percent of adult patients receiving any form of disease-modifying therapy.18,19 The lack of comprehensive sickle cell centres, limited access to specialty medical care, and persistent healthcare coverage gaps create substantial barriers for patients trying to manage their condition.
Despite the available therapeutic options, SCD remains significantly under-treated, with less than 30 percent of adult patients receiving any form of disease-modifying therapy.
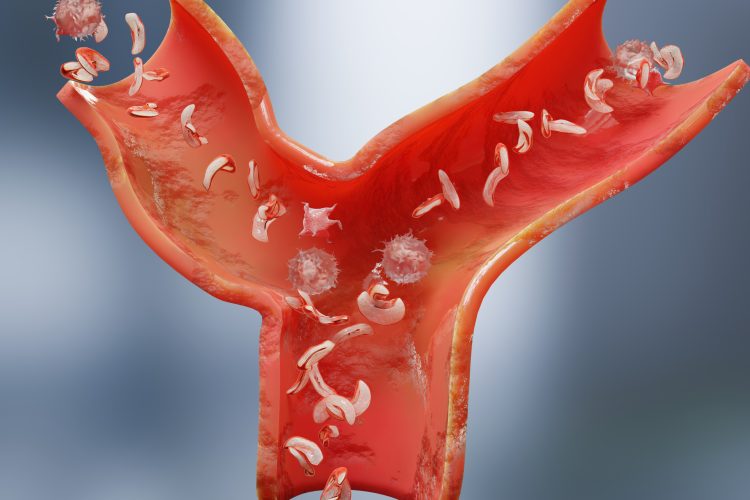
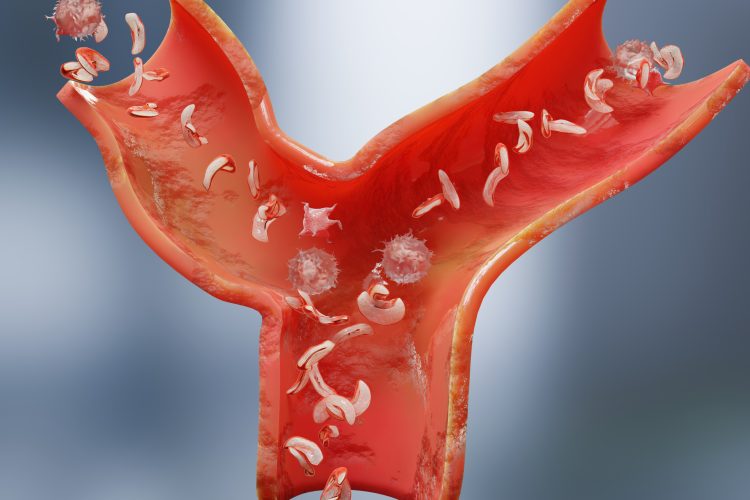
These gaps in SCD care are reflected in high healthcare resource utilisation, with 90 percent of adult SCD patients reporting at least one severe pain crisis and two-thirds experiencing three or more vaso-occlusive crises in the previous year.3,20 These crises drive high rates of emergency department use and hospital admissions, significantly disrupting education, employment and family life.3,20
Perhaps most glaring is that less than 2 percent of SCD patients in the US received RBCX treatment in 2022,18,19 despite significant evidence of its impact and potential. Studies presented at the American Society of Hematology 2024 Annual Meeting have predicted that patients receiving regular aRBCX would save up to $100,000 per patient lifetime to the healthcare system compared to other transfusion modalities, while increasing quality of life.22,23 Therefore, aRBCX was shown to have better clinical outcomes while providing cost savings. There was a predicted 21.5 percent reduction in the lifetime occurrence in vaso-occlusive events and a 5 percent reduction in the number of strokes. Even more striking, the model has demonstrated an eight-fold reduction in the need for chelation therapy (from 43 to five months compared to manual RBCX).22,23
These findings underscore that expanding access to aRBCX may lead to improved control of SCD in alignment with the World Health Organization’s (WHO’s) goal of achieving universal health coverage by integrating SCD treatments into existing healthcare programmes.
Expanding access and impact
A major step forwards came in February 2025 with the announcement of the BET on Blood for SCD partnership between the National Alliance of Sickle Cell Centers (NASCC) and Terumo Blood and Cell Technologies. This collaboration emphasises that blood is an essential therapy for managing SCD and aims to address critical gaps in access to blood transfusion therapy. The partnership is particularly timely given current disparities in care access, with surveillance data showing that 24 percent of children and 56 percent of adults with SCD did not see a haematologist over a three-year study period.24
Hospitals can also play a role, as shown by Harbor-UCLA Medical Center. Los Angeles County has more adults with SCD than anywhere else in California, making it an ideal and vital location for a treatment clinic. In 2018, Rachel Rangwala, MD, Director of Transfusion Medicine, led the establishment of a programme offering outpatient automated red blood cell-exchange transfusion therapy. Recently, the programme earned a prestigious Top 10 County of Los Angeles Productivity and Quality Award for developing innovative ways to empower vulnerable populations. Harbor’s use of RBCX resulted in better management of SCD patients’ pain crises, reduced emergency visits and hospitalisations, and improved patient quality of life while achieving significant Medicaid-related savings.21
The path forward requires key challenges to be addressed in infrastructure development, healthcare provider training, care coordination and cost coverage. Opportunities exist to leverage telemedicine and remote monitoring to support programmes in resource-limited settings, while partnerships between academic medical centres and community facilities can help build expertise.
Conclusion
As gene therapy moves towards broader availability, aRBCX will remain a crucial tool for mitigating complications and improving quality of life for the global SCD community.14,17 Through strategic partnerships like the NASCC initiative, we can work to ensure this vital therapy reaches all patients who need it, serving not only as a bridge to potential cures but as an essential component of comprehensive SCD care.
Meet the authors
Carly Newton, RN, MBA is the Senior Manager, Apheresis Clinical Marketing at Terumo Blood and Cell Technologies


Carly earned her Nursing degree at the University of South Australia and started her early career as a nurse in Australia, where she spent over a decade providing critical patient care, primarily in ICU settings. Carly transitioned to the medical device industry following her aspirations to improve patient outcomes through blood and cell technology. Specialising in apheresis treatments, Carly has over 20 years of experience helping Healthcare Professionals treat conditions such as sickle cell, with red blood cell exchange.
Aaron Haubner, PhD, MBA is the Senior Manager, North America Medical Affairs and Market Access at Terumo Blood and Cell Technologies


Aaron earned his doctorate in pharmaceutical sciences and his MBA in finance. Dr Haubner began his career in 1995 as a laboratory scientist, working on projects spanning molecular biology, cell culture and bioprocessing, drug design and discovery, high-throughput screening, and in-vitro diagnostics innovations. Since 2007 he has held senior positions in the medical device industry, managing a wide range of business units including: US sales and marketing, research and development, quality& regulatory, scientific, and medical affairs and market access. Dr Haubner regularly contributes to the field through original research, writing, speaking, and through his journal editorial activities.
References
- Mangla A, Ehsan M, Agarwal N, et al. Sickle Cell Anemia. [Updated 2023 Sep 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482164/
- Kayle M, Blewer AL, Pan W, et al. Birth Prevalence of Sickle Cell Disease and County-Level Social Vulnerability – Sickle Cell Data Collection Program, 11 States, 2016-
- Snyder AB, Lakshmanan S, Hulihan MM, et al. Surveillance for Sickle Cell Disease – Sickle Cell Data Collection Program, Two States, 2004-2018. MMWR Surveill Summ. 2022 Oct 7;71(9):1-18. doi: 10.15585/mmwr.ss7109a1. PMID: 36201430; PMCID: PMC9552568.
- Jiao B, Johnson KM, Ramsey SD, et al. Long-term survival with sickle cell disease: a nationwide cohort study of Medicare and Medicaid beneficiaries. Blood Adv. 2023 Jul 11;7(13):3276-3283. doi: 10.1182/bloodadvances.2022009202. PMID: 36929166; PMCID: PMC10336259.
- Newman TV, Yang J, Suh K, et al. Use of Disease-Modifying Treatments in Patients With Sickle Cell Disease. JAMA Netw Open. 2023 Nov 1;6(11):e2344546. doi: 10.1001/jamanetworkopen.2023.44546. PMID: 37991760; PMCID: PMC10665975.
- Cronin RM, Lin CJ, Chiang C, et al. The use of FDA-approved medications for preventing vaso-occlusive events in sickle cell disease. Blood Adv. 2023 Jul 11;7(13):3114-3116. doi: 10.1182/bloodadvances.2022008965. PMID: 36883847; PMCID: PMC10362533.
- Lesmana H, Kim SY, Corado AM, Poskanzer SA; ACMG Therapeutics Committee8∗[email protected]. Casgevy (exagamglogene autotemcel) and Lyfgenia (lovotibeglogene autotemcel) for individuals 12 years and older with sickle cell disease (SCD) and recurrent vaso-occlusive crises (VOC): A therapeutics bulletin of the American College of Medical Genetics and Genomics (ACMG). Genet Med Open. 2024 Sep 10;2:101875. doi: 10.1016/j.gimo.2024.101875.
- Michot J, Driss F, Guitton C, et al. Immunohematologic tolerance of chronic transfusion exchanges with erythrocytapheresis in sickle cell disease. Transfusion. 2014;55(2):357-363.
- Wahl SK, Garcia A, Gildengorin G, et al. Lower alloimmunization rates in pediatric sickle cell patients on chronic erythrocytapheresis compared to chronic simple transfusions. Transfusion. 2012;52(12):2671-2676.
- Lombardo T, Rosso R, La Ferla A, et al. Acute chest syndrome: the role of erythro-exchange in patients with sickle cell disease in Sicily. Transfus Sci. 2003;29(1):39-44
- National Institute for Health and Care Excellence. Spectra Optia for automatic red blood cell exchange in patients with sickle cell disease. https://www.nice.org.uk/guidance/mtg28. Medical technologies guidance (MTG28). Published March 2016.
- Singer T, Quirolo K, Nishi K, et al. Erythrocytapheresis for chronically transfused children with sickle cell disease: an effective method for maintaining a low HbS level and reducing iron overload. J Clin Apher. 1999;14(3):122-125.
- Kalff A, Dowsing C, Grigg A. The impact of a regular erythrocytapheresis programme on the acute and chronic complications of sickle cell disease in adults. Br J Haematol. 2010;149(5):768-774.
- Chou S, et al. American Society of Hematology 2020 guidelines for sickle cell disease: transfusion support. Blood Advances. 28 JANUARY 2020. VOLUME 4, NUMBER 2
- Sharma D, et al. Managing sickle cell disease and related complications in pregnancy: results of an international Delphi panel. Blood Adv(2024) 8 (4): 1018–1029.
- Asma S, Kozanoglu I, Tarım E, et al. Prophylactic red blood cell exchange may be beneficial in the management of sickle cell disease in pregnancy. Transfusion. 2015;55(1):36-44.
- Connelly-Smith, et al. Guidelines on the Use of Therapeutic Apheresis in Clinical Practice – Evidence-Based Approach from the Writing Committee of the American Society for Apheresis: The Ninth Special Issue. J Clin Apher. 2023, (38): 77-278
- Newman T, Yang J, Suh K, et al. Use of Disease-Modifying Treatments in Patients with Sickle Cell Disease. JAMA Network Open. 2023;6(11)
- Newman TV, Yang J, Haubner A, et al. 3690 Use of Chronic Blood Transfusions and Pharmaceutical Disease-Modifying Therapies in Sickle Cell Disease: A Retrospective Cohort Analysis (2014-2021). Presented at American Society of Hematology, Annual Metting, San Diego, CA, December 2024.
- Udeze C, Evans KA, Yang Y, et al. Economic and Clinical Burden of Managing Sickle Cell Disease with Recurrent Vaso-Occlusive Crises in the United States. Adv Ther. 2023 Aug;40(8):3543-3558. doi: 10.1007/s12325-023-02545-7. Epub 2023 Jun 18. Erratum in: Adv Ther. 2023 Nov;40(11):5130.
- Article, Terumo BCT website: [Award-winning program changes lives for patients with sickle cell disease in LA County].
- Cawson M, Medland S, Bainbridge J, et al. 5002 Clinical and Economic Impact of Long-Term Disease Modifying Transfusions in Paediatrics as a Prophylactic Intervention for Sickle Cell Disease Crises. Presented at American Society of Hematology, Annual Metting, San Diego, CA, December 2024.
- Cawson M, Medland S, Bainbridge J, et al. 5001 Clinical and Economic Impact of Long-Term Disease Modifying Transfusions in Adults as a Prophylactic Intervention for Sickle Cell Disease Crises. Presented at American Society of Hematology, Annual Metting, San Diego, CA, December 2024.
- Horiuchi S, Zhou M, Snyder A, Paulukonis. Hematologist encounters among Medicaid patients who have sickle cell disease. Blood Adv(2022) 6 (17): 5128–5131.
Related topics
Analysis, Antibodies, Disease Research, Drug Development, Gene Therapy, Precision Medicine, Research & Development, Translational Science
Related conditions
Sickle cell disease (SCD)