Advancing cell therapies with engineered Tregs
Posted: 10 September 2020 | Jason Fontenot (Sangamo Therapeutics) | 1 comment
Regulatory T cells (Tregs) play a key role in regulating our immune system and inflammatory processes. Sangamo Therapeutics is evaluating the potential of CAR-Tregs (Tregs genetically modified with a chimeric antigen receptor, or CAR) for the development of therapies for immunological diseases, such as Crohn’s disease and multiple sclerosis, as well as for the prevention of immune-mediated rejection in a solid organ transplantation setting. Jason Fontenot, Sangamo’s Senior Vice President of Cell Therapy and Interim Head of Research, discusses their approach and clinical pipeline.
Why are cell therapies of interest to researchers?
Engineered cell therapies are an incredibly exciting new therapeutic modality. They leverage the ability of cells to adapt to their environment, self-renew and persist after a single dose. They are living drugs. Cell therapies are being developed to treat many diseases – cancer, autoimmunity, monogenic diseases are all examples. They have the potential to address medical challenges and offer levels of therapeutic benefit that have not been possible with simpler therapeutic solutions (such as chemical drugs or antibodies). Recently, two genetically engineered T-cell (chimeric antigen receptor [CAR] T-cell) therapies have shown remarkable efficacy in the treatment of blood cancers and have been approved to treat those diseases.
Cell therapies can be broadly divided into two categories: the first is unmodified cells that are simply collected, selected and expanded, but not modified; the second, the type that we are focused on, are engineered cell therapies. These therapies use cells that have been genetically modified ex vivo (outside the body) to enhance their therapeutic potential and our zinc finger platform is uniquely well-suited for engineering cell therapies We are moving multiple therapies forward using different engineered cells and I am particularly excited about our engineered regulatory T cell (Treg) platform. We are engineering Tregs to add a CAR, which gives Tregs the ability to target specific molecules and tissues. We call these engineered Treg cells CAR-Tregs.
Why have you decided to focus on regulatory T cells?
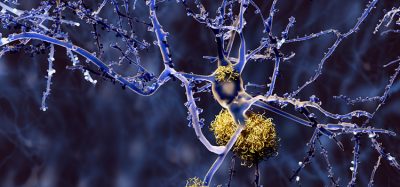
Tregs are a specific type of immune cell and are a sub-population of T cells. They are key regulators of our immune system and have a targeted immunosuppressive function. They inhibit inflammatory processes thanks to multiple mechanisms of action. Tregs have also been shown to promote tissue healing and regeneration. There is a substantial body of scientific literature demonstrating the therapeutic potential of Tregs; for instance, in mouse models of autoimmune and inflammatory diseases, Tregs have been demonstrated to prevent and even cure disease pathology. This curative potential, the ability to reset the body’s immune system to a normal, healthy state, is what is most exciting about engineered Treg cell therapies.
This curative potential, the ability to reset the body’s immune system to a normal, healthy state, is what is most exciting about engineered Treg cell therapies”
We like to describe Tregs as ‘peacekeepers’ because they can direct other immune cells to ceasefire and ensure they do not mistakenly attack healthy organs, whilst still allowing the immune system to protect the body from harm, such as against viruses and bacteria. Clinical trials in humans using unmodified Tregs have demonstrated that they can be safely used as cell therapies. Our approach is to enhance and target the Tregs to improve their therapeutic potential. We believe this approach has great promise for the treatment of many autoimmune and inflammatory diseases.
What are autologous cell therapies and how do they differ from other approaches?
An autologous cell therapy is made using cells from the person who will be the recipient of the cell therapy. Put simply, a patient’s cells are used as the therapy. The cells are isolated from a simple blood sample or by leukapheresis (a procedure to separate and collect white blood cells from a patient’s blood). We then engineer the patient’s cells into a cell therapy product and this is then injected back into the patients, for instance, intravenously. This is what we call an autologous cell therapy. In contrast, an allogeneic cell therapy is made using cells from a person other than the recipient of the cells, for instance a healthy donor.
Can you explain the cell engineering process to manufacture CAR-Treg cells?
For our first CAR-Treg candidate therapy, TX200, which targets transplant rejection, we are using a lentivirus to engineer the Treg cells to express the CAR. We are working on more advanced genetic engineering approaches for future CAR-Treg therapies. For these, we are using our proprietary zinc finger nuclease (ZFN) technology. Using this technology, we are developing additional enhancements to the Tregs to improve their properties and function.
Have you encountered any significant challenges during development?
A significant challenge with any engineered cell therapy is the development of a robust and efficient ex vivo process for isolating, engineering and expanding the cells. Tregs share some properties with other T cells and this has allowed us to build upon the learnings from the CAR-T cell field. On the other hand, Tregs have distinctive properties that have required that we innovate. They are a relatively rare cell population in circulation and the conditions to expand them are unique. We are investing significantly in developing an effective and scalable process for manufacturing our CAR-Treg cell therapies.
How do you expect the CAR-Treg cells to function following patient administration?
We are working on more advanced genetic engineering approaches for future CAR-Treg therapies”
After the intravenous injection, we expect that CAR‑Treg cells will accumulate and expand in the tissue that we have targeted with the CAR. For instance, if we take the example of kidney transplant, we have engineered the CAR-Tregs to recognise a molecule that is unique to the transplanted kidney. As we have seen in pre-clinical animal models, we expect that the CAR‑Tregs will proliferate, accumulate and become activated in the tissue targeted by the CAR, in this case the patient’s new kidney. In this way, we expect that they will exert their anti-inflammatory properties and prevent rejection of the kidney. We can generalise this approach for autoimmune diseases and different tissues. The CAR-Tregs should be able to reduce inflammation and inhibit immune‑mediated pathology in a targeted way. A very exciting aspect of the therapy is that the CAR-Tregs have the potential to persist for long periods of time and we hope that this will result in a durable therapeutic effect.
What conditions are you hoping to treat?
We are investigating CAR-Tregs in autoimmune and inflammatory diseases as well as in transplant rejection. Our first CAR-Treg programme, TX200, targets the prevention of immune‑mediated rejection following mismatched kidney transplantation. We also have other CAR-Treg programmes targeting autoimmune diseases such as multiple sclerosis and inflammatory bowel disease.
What is next?
We are working to initiate a clinical study named STEADFAST to evaluate TX200, our first CAR‑Treg programme, in patients who have received a mismatched kidney transplant. We hope that TX200 can help the patient’s body accept their transplanted kidney and prevent immune-mediated graft rejection. The STEADFAST study will help us understand how TX200 works in humans and may provide broader proof-of-concept for genetically modified cell therapy using Tregs. So far, our clinical trial application (CTA) has been approved in the UK and we are working towards other regulatory approvals. The next step will be to initiate first clinical sites in Europe.
About the author
Jason Fontenot has been assuming the role of Interim Head of Research at Sangamo since June 2020. He has served as Sangamo’s Senior Vice President of Cell Therapy since March 2019 where he oversees Sangamo’s engineered cell therapy portfolio. This includes a proprietary chimeric antigen receptor regulatory T cell (CAR-Treg) pipeline, a partnership with Sanofi focused on ex vivo genome editing programmes in haemoglobinopathies and a partnership with Kite, a Gilead Company, to develop autologous and allogeneic CAR-T cell therapies in oncology. Jason has an extensive background in cell therapy and drug development, having previously served as Chief Scientific Officer at Immusoft, Head of Exploratory Research at Juno Therapeutics and for nearly a decade as a group leader in the immunology department at Biogen. Jason conducted post-doctoral work at Rockefeller University in New York City. He received his PhD in Immunology from the University of Washington in Seattle working in the laboratory of Alexander Rudensky.
Related topics
Biopharmaceuticals, Drug Development, Immuno-oncology, Immunotherapy, Research & Development, T cells, Therapeutics
Related conditions
autoimmune diseases, Cancer, Crohn’s disease, Multiple Sclerosis (MS), organ transplants
Related organisations
Bio-Rad








Nikki, thank you for sending me this great article. Dr. Carl Edwards