The next generation of cancer immunotherapies: re-exploring the IL-2 pathway
Posted: 17 September 2020 | Dr Bruce Dezube (Alkermes) | No comments yet
In this article, Dr Bruce Dezube explains why new cancer immunotherapy drugs that utilise the IL-2 pathway with lower side effects could offer more benefits compared to high-dose IL-2 treatment.
As an oncologist for the past 34 years, I have seen how the cancer treatment landscape has evolved. In the early days, these treatments primarily included three modalities: chemotherapy, with only a handful of options; radiation therapy; or surgery. There were no targeted therapies available. However, over the years, we have seen incremental improvements in treatment options – until more recently when immunotherapies, such as checkpoint inhibitors, took centre stage and revolutionised the way that cancer is treated.
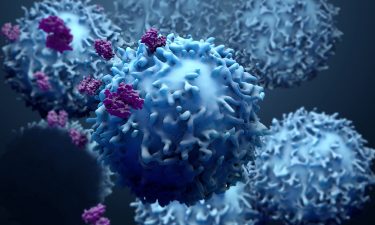
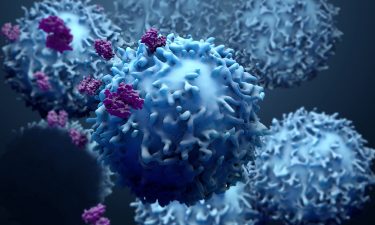
The advent of these immunotherapy approaches significantly improved clinical outcomes in many cancer types. However, immune checkpoint inhibitors are not an option for all cancer types: pancreatic and ovarian cancer, as well as most haematologic malignancies, do not have approved immuno-oncology (IO) options. Furthermore, many patients with cancer do not benefit from immunotherapies; for example, the response rates for single-agent immune checkpoint inhibitors in ovarian cancer is only ~six to 15 percent.1 Even patients with cancer types eligible for IO who respond initially may develop resistance after treatment.2,3 Suboptimal CD8+ T-cell response and activity of immune suppressive regulatory T cells are believed to be the key drivers of this resistance.4,5
Therefore, optimising the ability of cancer-fighting T cells and countering the effects of Tregs continue to be an active area of research today as companies attempt to develop the next generation of IO treatments. In doing this, numerous companies are revisiting previously existing therapies, such as interleukin-2 (IL-2), to develop potential new IOs.
History of IL-2 as a cancer therapy
In 1976, a T-cell growth factor – which later became known as IL-2 – was identified.5 Soon afterward, IL-2 was extensively studied in research laboratories. The first trial of purified IL-2 in patients with solid tumours (melanoma, sarcoma, adenocarcinoma and Kapsosi’s sarcoma) began in 1983, but while a few side effects were observed, no antitumour activity occurred.6,7
Challenges of IL-2 in clinical use
…optimising the ability of cancer-fighting T cells and countering the effects of Tregs continue to be an active area of research today”
A key challenge of using IL-2 in the clinic lies in its two receptors: the intermediate affinity and high affinity receptors.8 Binding to the intermediate affinity receptor, expressed primarily on CD8+ T cells and NK cells, drives antitumour activity; thus, for IL-2 therapies to be effective, they must activate this receptor. However, IL-2’s binding to its high affinity receptor, expressed on Tregs, suppresses immune responses including antitumour, by expanding these cells. Since the high affinity receptor binds IL-2 more potently than the intermediate affinity receptor, a low dose of IL-2 binds primarily to the high affinity receptor on Tregs without effectively activating CD8+ T cells and NK cells. A high dose of IL-2 is therefore needed to effectively activate these cancer-fighting cells expressing the intermediate affinity receptor; however, a high dose of IL-2 has also been reported to preferentially expand Tregs.9 Besides immune suppression via Tregs, IL-2 therapy has been associated with toxicities including capillary leak syndrome, which is believed to be driven by vascular endothelial cells that express the high affinity receptor.15
Therefore, preferential activation of the intermediate affinity receptor at a low dose has been the challenge that pharma companies are aiming to address with new, investigational IL-2 products.
The IL-2 renaissance: why companies are revisiting this pathway
Drug discovery is a long, arduous and cost-intensive journey, so shortening that timeframe and increasing the likelihood of finding a new treatment is incredibly important for cancer patients who are out of other options. The IO revolution has shown that improving the ability of T cells to fight cancer is a viable option. Accordingly, this provides strong rationale for revisiting the validated IL-2 pathway to see whether its cancer fighting arm can be selectively engaged by designing molecules that specifically target the intermediate-affinity receptor.
Modified IL-2 as a potential solution
Since Tregs are key players in treatment resistance and tumour escape, shifting the balance of T cells to reduce the activity and ratio of Tregs within the patient’s body has important implications for cancer treatment.10,11 Modified IL-2s are designed to preferentially bind the immunostimulatory, intermediate-affinity IL-2 receptor on antitumour CD8+ T cells and NK cells instead of the immunosuppressive, high affinity IL-2 receptor on Tregs.
Pegylated IL-27
Tumour-directed IL-27
Another approach for redesigning IL-2 involves fusing IL-2 to an antibody that targets a common tumour antigen, such as carcinoembryonic antigen or fibroblast activating protein. The IL-2 used in this approach must be mutated to prevent binding to the high affinity receptor.
IL-2/IL-2Ra fusion7,12
An additional strategy for modifying IL-2 rather uses circular permutation, a naturally occurring protein rearrangement process, to fuse IL-2 with the alpha chain of the high affinity IL-2 receptor. When the alpha chain is fused to IL-2, the resulting investigational drug can no longer bind the high affinity IL-2 receptor on Tregs and may only bind to the intermediate affinity receptor on antitumour CD8+ T cells and NK cells.
At Alkermes, we have harnessed circular permutation to pursue the development of a novel cytokine, re-engineered from IL-2, that is designed to selectively expand tumour-killing immune cells while avoiding activation of immunosuppressive cells.
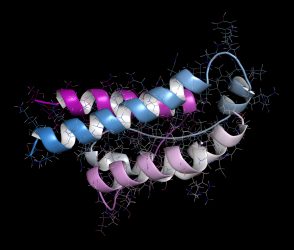
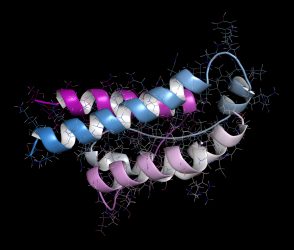
Interleukin-2.
This fusion protein design may offer several advantages. It is an inherently active drug candidate that may not need metabolic breakdown to be activated within the body. It is a highly stable molecule, mitigating concerns about it breaking down into the native form of IL-2, which could bind the high affinity receptors. Furthermore, this novel design is intended to allow for both intravenous and subcutaneous administration, potentially providing optionality for patients. The selectivity, efficacy and safety of this fusion protein are currently being investigated in clinical trials.
The IL-2 pathway has already proven to be a validated therapeutic target in oncology. The development of potential new drugs that leverage the proven clinical benefits of targeting this pathway, with lower side effects, could offer a significant improved benefit to risk profile compared to high-dose IL-2 treatment. In addition, early clinical and pre-clinical data suggest that newer IL-2 variant immunotherapies may be an appropriate addition to multiple other treatment approaches, enhancing their potential role in patient treatment.
About the author
Dr Bruce Dezube is an Executive Medical Director at Alkermes Inc., leading the company’s oncology clinical programme. Bruce has spent the last 10 years in the pharmaceutical industry in various clinical leadership roles, running large scale oncology clinical programmes. Prior to joining the industry, he served as Associate Professor of Medicine at Harvard Medical School. He has been part of several NIH/National Cancer Institute (NCI)-led consortiums and has received numerous awards and recognitions for his contributions to clinical oncology.
References
- Doo D, et al. Gynecol Oncol Rep. 2019; 29:48-54.
- de Erauso L, et al. Front. Pharmacol. 2020; doi: 10.3389/fphar.2020.00441.
- Jenkins R, et al. British Journal of Cancer. 2018; 118:9-16.
- Nowicki T, et al. Cancer J. 2018; 24(1): 47-53.
- Liu D, et al. American Journal of Clinical Dermatology. 2019 Feb; 20(1): 41–54.
- Rosenberg S. J Immunol. 2014; 192(12):5451-5458.
- Lotze M, et al. J Immunol. 1985; 134:157-166.
- Tang A and Harding F. Cytokine: X. 2019; 1:100001.
- Sim G, et al. J Clin Invest. 2014; 124(1):99-110.
- Verma A, et al. Cancer Manag Res. 2019; 11:10731-10747.
- Han S, et al. Front. Oncol. 2019; doi.org/10.3389/fonc.2019.00279.
- Lopes J, et al. J Immunother Cancer. 2020; 8(1):e000673.
- Clement J and McDermott D. Clin Genitourin Cancer. 2009;7(2):E7-9.
- Amaria R, et al. Immunotargets Ther. 2015;4:79-89.
- Krieg C, et al. Proceedings of the National Academy of Sciences. 2010; 107(26):11906-11.
Related topics
Drug Targets, Immuno-oncology, Immuno-oncology therapeutics, Immunotherapy, Oncology, Research & Development, Targets
Related conditions
Cancer
Related organisations
Alkermes








