Broad T-cell responses: designing a rhinovirus vaccine
Posted: 31 March 2021 | Nikki Withers (Drug Target Review) | No comments yet
The multiple serotypes of rhinovirus have presented difficulties for vaccine developers. Now, a team led by Professor Gary McLean from London Metropolitan University and Imperial College London, alongside Professor Sebastian Johnston from Imperial, has formulated a potential vaccine. Nikki Withers spoke to McLean to discover how the vaccine works and the promising results it showed in pre-clinical studies.
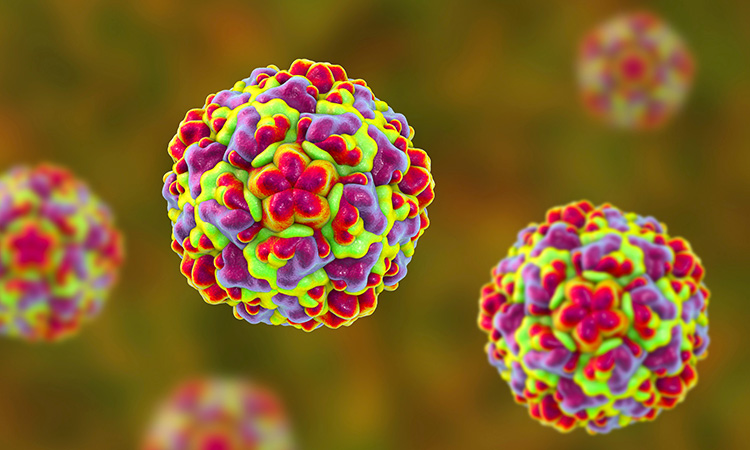
There are 160 different serotypes or strains of rhinovirus, making the development of a vaccine extremely challenging, according to McLean. Due to this high number of viral variants, the traditional technique of injecting an inactivated form of the virus to induce immunity is physically impossible and could not be administered to patients. To address this issue, McLean and the research team investigated how to find one aspect that is common to as many serotypes of rhinovirus as possible and use that to develop a recombinant subunit vaccine.1
The team focused on the well-characterised type A and type B rhinoviruses, of which there are approximately 100 known strains, using a bioinformatics approach. When the researchers began their study, a third group of rhinoviruses, type C, had only just been discovered and due to the limited information available was therefore excluded from their research.
Why study rhinoviruses
“The virus itself is very simple… it is just a shell of protein, so has a very simple structure and does not carry a large amount of genetic material,” said McLean. “The only way of fighting it, due to its speed, is to have immunity beforehand. Hence why a vaccine would be really wonderful.”
McLean emphasised that the importance of investigating potential vaccines against rhinoviruses is not because of the threat they pose once the host is infected, but the speed at which they move through populations. He explained that the virus is constantly evolving, with all strains circulating at all times.
“We found an area of type A and B that was very highly conserved or shared between all the strains. Named VP4, it is one of the capsid proteins. The capsid on the surface of the virus is made up of four different proteins: VP1, 2, 3 and 4,” explained McLean. He added that the 1, 2 and 3 capsid proteins tend to be found on the outside of the virus, whereas the VP4 capsid protein is found underneath. The researchers hypothesised that if presented with an antigen or immunogen not on the surface of the virus, antibodies would not be able to bind to the virus and neutralise it, which might allow more broadly suitable T-cell immunity to develop.
The challenge of antibodies
For rhinoviruses, antibodies correlate well to a certain level of protection, but are restricted to specific serotypes”
McLean highlighted that for rhinoviruses, antibodies correlate well to a certain level of protection, but are restricted to specific serotypes.
“The virus is very clever in that the external parts of the virus, which favour antibody binding and therefore neutralisation by antibodies, are frequently mutated. Every different strain has a new loop or a few different amino acids so that all the antibodies that bind to type A are completely useless against type B and even to many of the more distant type A,” he explained.
Having discovered that the internal VP4 was very highly conserved, McLean and the team suggested that this could instead be used to induce a T-cell response. This would provide robust protective immunity against more strains. “At this point, we knew we could forget about the antibodies and focus on a T-cell vaccine,” said McLean.
He explained that the target patient group for the potential rhinovirus vaccine the team developed would be people who typically exhibit a Th2 immune response associated with chronic lung conditions. The vaccine that the team are developing instead promotes Th1 immune responses to enable patients’ immune systems to recognise different rhinoviruses.
Developing the vaccine
The team initially made their recombinant protein that could be administered to induce an immune response. However, to gauge its success, they needed to develop a new model to assess the efficacy of the protein. Together with Imperial College London and Sanofi Pasteur, the team created a mouse model for their pre-clinical studies.
 “After developing the mouse model, we were the only ones in the world that could infect mice with rhinovirus. There was no small animal model at that point,” said McLean. He highlighted that the researchers required this model for their challenge studies, to test whether or not the immunity of the mice would be protective following administration of the prophylactic.
“After developing the mouse model, we were the only ones in the world that could infect mice with rhinovirus. There was no small animal model at that point,” said McLean. He highlighted that the researchers required this model for their challenge studies, to test whether or not the immunity of the mice would be protective following administration of the prophylactic.
However, McLean emphasised that the challenge when using the mouse models was that they could only infect them with four serotypes out of the 100. He explained that it was very difficult to establish the model because the virus had to be at an extremely high level when presented in the noses of the mice. Unlike human cells, rhinoviruses do not highly replicate in mouse cells, meaning that high levels of the virus had to be administered to the mice. Nonetheless, the researchers were able to create their model, which they published in a separate paper in Nature Medicine.2
Testing the vaccine
Once the researchers had developed their model and recombinant vaccine, they tested their immunisation strategy. According to McLean, the mice had excellent immune responses. They found that the mice generated a robust T-cell immune reaction with a favourable Th1 response because the vaccine was formulated with an effective adjuvant.
“To make the recombinant protein more immunogenic, we used a very strong Th1 polarising adjuvant,” McLean explained. This meant the immune responses of the mice were focused on CD4+ interferon‑gamma‑producing T cells. “When we took those cells out of the mice and cultured them in the presence of different rhinovirus antigens, those cells grew and started making lots of interferon-gamma, which was our readout.”
The mice generated a robust T-cell immune reaction with a favourable Th1 response because the vaccine was formulated with an effective adjuvant”
The researchers immunised the mice with one particular strain of the immunogen, which was conserved. They then challenged the mice with different strains of rhinovirus to investigate their immune response to different serotypes.
“Although these were just peptides, it provided a proof-of-concept that we could generate protective T-cell immunity to multiple serotypes of rhinovirus,” said McLean. “Surprisingly, we also found strong antibody responses that could offer protection but these were more serotype-specific than the T cells and we are still trying to establish why this is the case.”
The next steps
“We wanted to recreate everything we had done with a vaccine formulation that could go straight into people and demonstrate that instead of cross, broad protection against few rhinoviruses, we could go for many more,” said McLean.
Having obtained a US patent for their immunisation technique, called generation of cross‑serotype T-cell protective immunity, the team are now planning their next steps for development.
The researchers are also focusing on generating a much broader coverage, including investigating responses to type C rhinoviruses. They are additionally studying different adjuvants that would be better tolerated in humans, as the one used in the study would generate high toxicity if used clinically.
Nonetheless, McLean is focused on getting this potential vaccine to human clinical trials. “This potentially has huge positive outcomes for human health,” he concluded.
Extra Reading
Williams G, Kubajewska I, Glanville N, Johnston S, Mclean G. The potential for a protective vaccine for rhinovirus infections. Expert Review of Vaccines. 2016;15(5):569-571.
 Professor Gary McLean is an academic research scientist with over 25 years of experience in molecular studies of immune responses to human pathogens, developing significant ties with biotechnology and vaccine companies. His scientific training led him around North America, where he studied antibody gene diversification, produced unique monoclonal antibodies and began to develop viral vaccines. He is now based in London, UK, where his research focuses on structure-guided vaccine design for human viruses.
Professor Gary McLean is an academic research scientist with over 25 years of experience in molecular studies of immune responses to human pathogens, developing significant ties with biotechnology and vaccine companies. His scientific training led him around North America, where he studied antibody gene diversification, produced unique monoclonal antibodies and began to develop viral vaccines. He is now based in London, UK, where his research focuses on structure-guided vaccine design for human viruses.
References
- Glanville N, Mclean G, Guy B, Lecouturier V, Berry C, Girerd Y, et al. Cross-Serotype Immunity Induced by Immunization with a Conserved Rhinovirus Capsid Protein. PLoS Pathogens. 2013;9(9):e1003669.
- Bartlett N, Walton R, Edwards M, Aniscenko J, Caramori G, Zhu J, et al. Mouse models of rhinovirus-induced disease and exacerbation of allergic airway inflammation. Nature Medicine. 2008;14(2):199-204.
Related topics
Antibodies, Immunology, In Vivo, Vaccine
Related conditions
rhinovirus
Related organisations
GenScript, IDBS, Imperial College London, London Metropolitan University, Sanofi Pasteur
Related people
Professor Gary McLean, Professor Sebastian Johnston