Promising potential therapeutic strategy against pancreatic cancer developed
Posted: 24 March 2022 | Ria Kakkad (Drug Target Review) | No comments yet
Scientists have discovered a new strategy that can make pancreatic tumours visible to the immune systems of mice and vulnerable to immune attack.
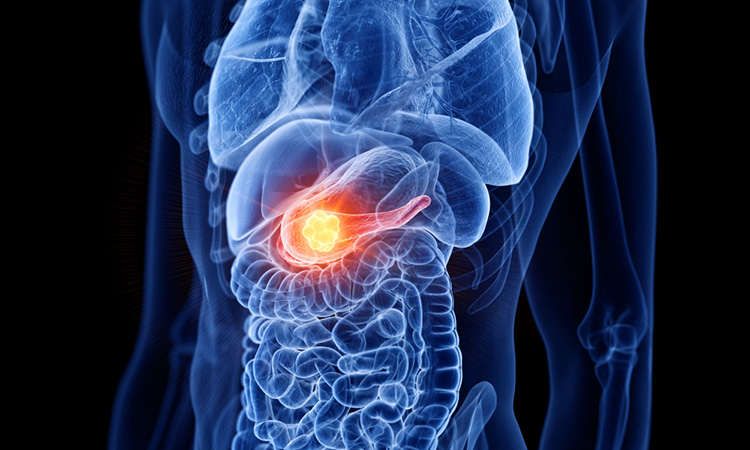
Scientists at the Albert Einstein College of Medicine, US have succeeded in making pancreatic tumours visible to the immune systems of mice and vulnerable to immune attack, reducing cancer metastases by 87 percent. The findings, recently published in Science Translational Medicine, represent a step towards a potential therapy against pancreatic cancer.
In their research, the team aimed to leverage a vaccine against tetanus, a serious disease caused by a toxic protein that Clostridium bacteria secrete. The tetanus-specific memory T cells in the tetanus vaccine circulate in the bloodstream for life, therefore vaccinated people will mount a strong immune response if they are later exposed to the highly foreign tetanus toxin. In their study, the researchers effectively aroused a potent and specific immune response against pancreatic cancer cells by infecting them with bacteria that deliver tetanus toxin into the cells.
Using the same common tetanus vaccine, the investigators vaccinated mouse models of pancreatic cancer. They then fused the gene that codes for tetanus toxin into Listeria monocytogenes, a bacterium that does not cause disease but are highly adept at infecting cells and spreading through tissues. Finally, to infect and “tetanise” the tumours, they injected the bacteria with their tetanus-gene cargoes into the previously vaccinated, tumour-bearing mice.
“The Listeria bacteria are quite weak and are readily killed off by the immune systems of people and animals — everywhere, that is, except in tumour areas,” said Dr Claudia Gravekamp, corresponding author of the paper and Associate Professor of Microbiology and Immunology. “Our treatment strategy actually takes advantage of the fact that pancreatic tumours are so good at suppressing the immune system to protect themselves. This means that only those Listeria bacteria in the tumour region survive long enough to infect pancreatic tumour cells and that healthy cells do not become infected.”
Once the Listeria bacteria infected the tumour cells, their tetanus-toxin genes expressed the tetanus-toxin protein inside the tumour cells, triggering a strong immune response. The tetanus toxin activated pre-existing tetanus-specific memory T cells, causing CD4 T cells to attack and kill the infected tumour cells. The T-cell responses were enhanced by adding low doses of gemcitabine, a chemotherapy drug that reduces immune suppression. The treatment shrank the size of the pancreatic tumours in the mice by an average of 80 percent and significantly reduced the number of metastases by 87 percent. In addition, the treated animals lived 40 percent longer than untreated animals.
“The findings indicate that this treatment approach could be a useful immunotherapy for pancreatic cancer as well as other types of cancer, such as ovarian cancer, that remain difficult to treat,” concluded Dr Gravekamp.
Related topics
Chemotherapy, Disease Research, Drug Repurposing, Immuno-oncology, Immuno-oncology therapeutics, Immunotherapy, Vaccine
Related conditions
Pancreatic cancer
Related organisations
Albert Einstein College of Medicine
Related people
Dr Claudia Gravekamp