FGF19 hormone could be the key to new obesity treatments
Posted: 4 July 2025 | Drug Target Review | No comments yet
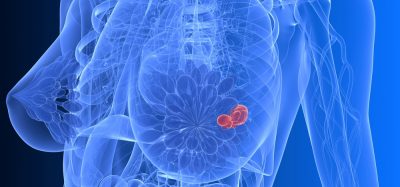
A hormone produced in the gut, FGF19, has been shown to act directly on the brain to boost energy expenditure, burn fat and improve blood sugar control in obese mice – offering a potential route for developing new obesity therapies.
New research conducted at the State University of Campinas (UNICAMP) has revealed that a hormone released by the small intestine – fibroblast growth factor 19 (FGF19) – plays a direct role in controlling the body’s energy expenditure by acting on the brain. The findings show that FGF19 can help stimulate fat burning, improve blood glucose levels and regulate body weight in obese mice models.
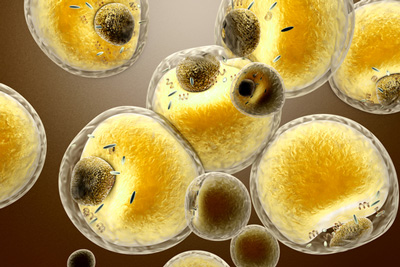
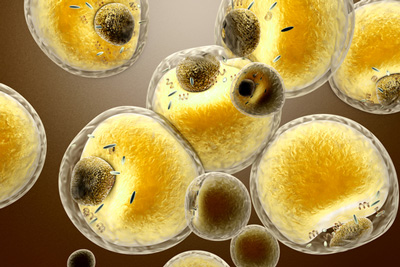
The study, published in the American Journal of Physiology – Endocrinology and Metabolism, identified the hormone’s activity in the hypothalamus – a key brain region responsible for integrating environmental and physiological signals. There, FGF19 triggers thermogenic activity in adipocytes – fat cells that burn energy to produce heat.
A potential therapeutic avenue
This new discovery could lead to a new line of obesity and diabetes treatments based on substances that mimic naturally occurring hormones like FGF19. It mirrors the success of therapies such as semaglutide – sold under the brand name Ozempic – which mimics the GLP-1 hormone to signal satiety and aid weight loss.
“FGF19 had already been linked to a reduction in food intake. Our work broke new ground by showing that it also plays an important role by acting on the hypothalamus and stimulating an increase in energy expenditure in white and brown adipose tissue. In other words, in addition to controlling appetite, it stimulates thermogenesis. So, in terms of therapy associated with obesity, it’d make a lot of sense,” said Professor Helena Cristina de Lima Barbosa, from the Obesity and Comorbidities Research Center (OCRC) at the State University of Campinas (UNICAMP).
Cold response and inflammation control
The study further found that FGF19 reduced peripheral inflammation and improved cold tolerance – effects that vanished when the sympathetic nervous system was inhibited. Cold exposure was shown to increase the expression of FGF19 receptors in the hypothalamus, highlighting the hormone’s role in thermoregulation.
“The brain plays an extremely important role in controlling the body’s adiposity. At the same time as it receives information from peripheral tissues, it triggers commands. These commands, apparently using the sympathetic nervous system, seem to be an interesting way of thinking about energy expenditure,” Barbosa explained.
Step-by-step findings
FGF19 is primarily produced in the small intestine and is already known for its role in the liver – where it regulates bile acids and the synthesis of glucose and fats. However, its signalling in the brain remained underexplored.
FGF19 is primarily produced in the small intestine and is already known for its role in the liver – where it regulates bile acids and the synthesis of glucose and fats.
“In the lab, we work with bile acids, which are also the subject of my master’s degree, and they regulate the release of FGF-19. Our initial studies led us down this path,” said Lucas Zangerolamo, a doctoral student at UNICAMP and first author of the study.
In the study, mice were divided into two groups – one receiving a regular diet and the other a high-fat diet. FGF19 was then administered directly into the brains of the obese mice. This central signalling improved energy homeostasis by activating the sympathetic nervous system and increasing energy-burning thermogenesis in adipose tissue.
The research also utilised public single-cell RNA sequencing (scRNA-seq) data, analysing more than 50,000 cells to map which hypothalamic cell types express FGF19 receptors.
A global health imperative
The World Atlas of Obesity 2025 reports that more than 1 billion people worldwide are currently living with obesity – a number that could surpass 1.5 billion by 2030 without effective interventions. Obesity contributes to 1.6 million premature deaths each year through its links to chronic conditions such as heart disease, diabetes and cancer.
Looking ahead
The research team, supported by the São Paulo Research Foundation (FAPESP), continues to investigate how the body’s natural production of FGF19 can be enhanced and how it may influence inflammation in the hypothalamus linked to high-fat diets.
“We want to broaden this understanding,” said Zangerolamo. “We’re studying the hypothalamus to evaluate the inflammation commonly observed when a high-fat diet is administered and whether FGF19 plays a role in this area.”
Related topics
Animal Models, Central Nervous System (CNS), Drug Targets, Hormones, Molecular Biology, Neurosciences, Obesity, Therapeutics
Related conditions
Obesity
Related organisations
Sao Paulo Research Foundation – FAPESP, the State University of Campinas (UNICAMP)