Immunotherapy could cure advanced pancreatic cancer
Posted: 11 October 2018 | Iqra Farooq (Drug Target Review) | No comments yet
Immunotherapy using ‘educated’ killer cells could be a potential cure for pancreatic cancer, with researchers eliminating all signs of cancer from mice…
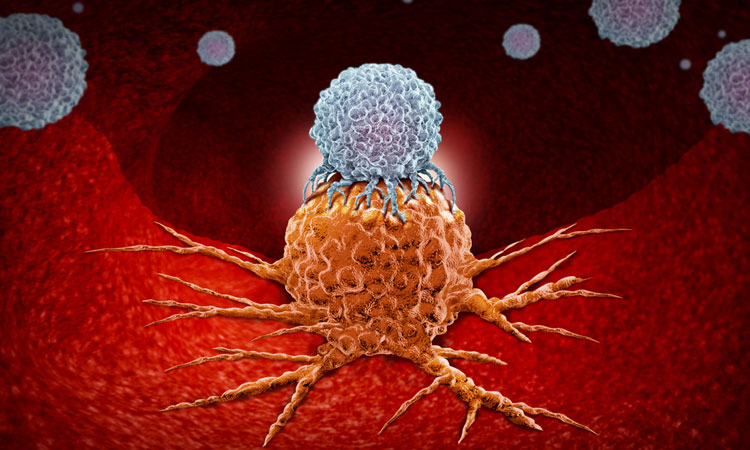
Researchers at Queen Mary University of London have developed an approach to treat pancreatic cancer using ‘educated’ killer cells.
In vivo tests resulted in mice being completely cancer-free. The researchers mentioned that even cancer cells that had spread to the liver and the lungs were killed. The new therapy has not yet been tested in humans.
The researchers used pancreatic cancer cells from humans with late-stage pancreatic cancer. They transplanted these cells into the mice. the patients own immune cells were modified to specifically identify and eliminate the cancer cells. These modified cells, labelled as ‘educated’ killer cells, also known as CART-T cells.
Biomarkers aren’t just supporting drug discovery – they’re driving it
FREE market report
From smarter trials to faster insights, this report unpacks the science, strategy and real-world impact behind the next generation of precision therapies.
What you’ll unlock:
- How biomarkers are guiding dose selection and early efficacy decisions in complex trials
- Why multi-omics, liquid biopsy and digital tools are redefining the discovery process
- What makes lab data regulatory-ready and why alignment matters from day one
Explore how biomarkers are shaping early drug development
Access the full report – it’s free!
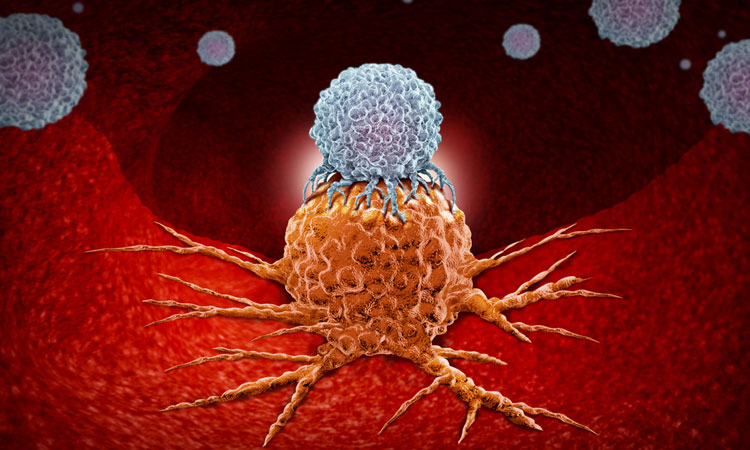
Dr Deepak Raj, first author of the study, at Queen Mary University of London, said: “Immunotherapy using CAR-T cells has been tremendously successful in blood cancers, but unfortunately, there have been toxic side effects in its treatment of solid tumours. Given the dismal prognosis of pancreatic cancer with conventional treatments, it’s vitally important that we develop safe and effective CAR-T cell therapies for solid tumours, such as pancreatic cancer.”
The team also introduced a technology that allowed the complete control of the CART-T cell activity, which potentially makes them safer.
“Our work suggests that our new ‘switchable’ CAR-T cells could be administered to human patients with pancreatic cancer, and we could control their activity at a level that kills the tumour without toxic side effects to normal tissues.”
As the treatment is ‘switchable’. the researchers can turn the therapy on or off, or change the activity to a desired level. They suggest that this would make the therapy safer and would minimise side effects, and would be controlled through the administration or the withdrawal of a switch molecule in the living mice.
Nile Amos, Research Manager at Pancreatic Cancer UK, said: “We are proud to have funded this research which highlights the potential of CAR-T cell immunotherapy for taking on pancreatic cancer. For more than 40 years too little progress has been made on developing new treatments for this devastating disease, for which survival remains unacceptably low.
“The results are extremely promising but there is more work to be done, which is why we are delighted to be funding the next stage of this cutting-edge science through our largest ever research grant, the Pancreatic Cancer UK Grand Challenge Award.”
The researchers hope to bring the therapy to the clinic to help patients.
The study was published in the journal Gut.
Related topics
Disease Research, Drug Discovery, Drug Discovery Processes, Immunotherapy, In Vivo, Oncology, Research & Development, Therapeutics
Related conditions
Pancreatic cancer
Related organisations
Queen Mary University of London
Related people
Dr Deepak Raj, Nile Amos