Removing macrophages shows success against ovarian cancer in mice
Posted: 27 March 2020 | Victoria Rees (Drug Target Review) | No comments yet
By removing two kinds of macrophages in mice, researchers showed that ovarian tumours in mice were reduced in size and stopped spreading.
A new study has demonstrated that it is possible to hinder the spread of ovarian cancer and reduce tumour size in mice.
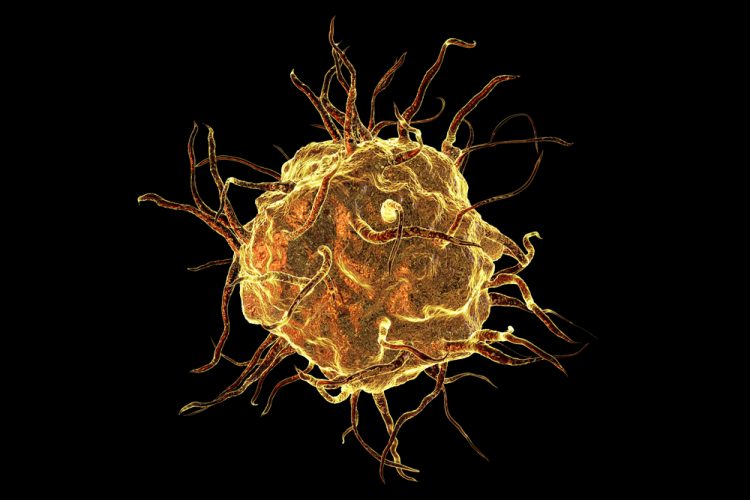
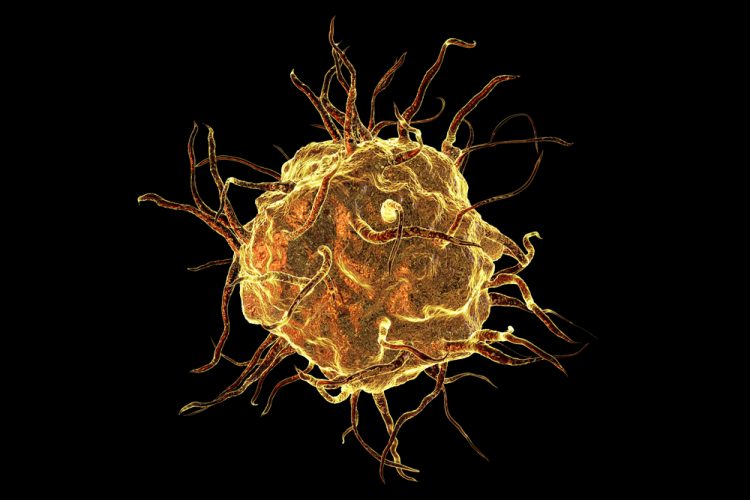
The researchers, led by scientists at Aarhus University, Denmark, removed some specific immune cells, known as macrophages, from the fat that is stored in the abdominal cavity and hanging in front of the intestines, known as omental fat.
“This is where the omental fat becomes a kind of host for cells which would otherwise perish and our research now shows that when tumour cells move into the omental fat, two specific types of immune cell known as macrophages alter character. They develop into the disease’s small supporters,” said lead researcher Dr Anders Etzerodt, assistant professor of cancer immunology at the Department of Biomedicine at Aarhus University. The researchers explain that ovarian cancer most often occurs in the fallopian tubes and that the starting point for the project was familiar knowledge about cancer cells being able to detach and shed into the abdominal cavity. As this occurs very early in the course of the disease, the ‘homeless’ cancer cells need to fasten onto something to survive.
“One of the macrophage types which is already present in the tissue simply begins to help the tumour spread further to the other organs in the abdominal cavity. At the same time, the second type of macrophage, which comes from the bloodstream and is recruited as a reaction to the infiltration of tumour cells into the omental fat, begins to counteract the immune system’s attempt to fight the invasive cancer cells. In this way, they help the tumour to grow larger.”
This project is only the third scientific article to describe how macrophages with different origins affect tumour development”
The researchers experimented with removing the macrophages already found in the tissue, which led them to establish that this inhibited the spread of cancer in the abdominal cavity – though without the tumour in the omental fat becoming smaller. When the researchers simultaneously removed the first type of macrophage mentioned above from the bloodstream, the result was both less spreading and a shrinking tumour.
“We describe a type of immunotherapy which differs from the immunotherapy that is characterised by supporting the T cells that kill a tumour and which has become an established part of modern immunological treatment,” commented Etzerodt. “What we’re doing is also immunotherapy, but it focuses on another part of the immune system. This project is only the third scientific article to describe how macrophages with different origins affect tumour development and precisely how the macrophages that are found to inhibit the immune system’s ability to hamper the cancer can be removed.”
The researchers also found the new types of macrophages using a new technique called single-cell sequencing, a method which gives the researchers very detailed information about the processes that take place in each individual cell.
According to Etzerodt, their results have obvious potential for improved treatment in the future; the next step is to develop a medicine which can be tested on people. This is particularly interesting, say the researchers, because the group has previously shown that similar macrophages from the bloodstream are also present in models for skin cancer.
“So far, we’ve gained a new and deeper understanding of what is helping and what is hindering the body in the development of ovarian cancer and I’m looking forward to testing this in clinical trials on patients who currently have a really poor prognosis,” Etzerodt said.
The study was published in the Journal of Experimental Medicine.
Related topics
Drug Targets, Immuno-oncology, Immunology, Immunotherapy, Research & Development, Targets
Related conditions
Ovarian cancer
Related organisations
Aarhus University
Related people
Dr Anders Etzerodt