Analysis of immune response to SARS-CoV-2 gives hope for COVID-19 vaccines
Posted: 19 May 2020 | Victoria Rees (Drug Target Review) | No comments yet
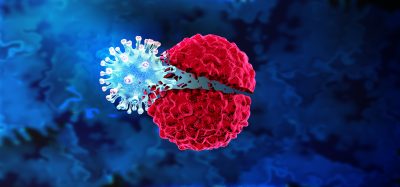
A detailed analysis of the body’s immune response to COVID-19 has revealed that it can recognise SARS-CoV-2 in many ways, meaning vaccines can be used to stop the spread of the virus.
A group of researchers from La Jolla Institute for Immunology, US, has studied the robust antiviral immune response to SARS-CoV-2 in a group of 20 adults who had recovered from COVID-19. According to the scientists, the findings show that the body’s immune system is able to recognise SARS-CoV-2 in many ways, dispelling fears that the virus may elude ongoing efforts to create an effective vaccine.
“If we had seen only marginal immune responses, we would have been concerned,” said Dr Alessandro Sette, a professor in the Center for Infectious Disease and Vaccine Research. “What we see is a very robust T-cell response against the Spike (S) protein, which is the target of most ongoing COVID-19 efforts, as well as other viral proteins. These findings are really good news for vaccine development.”
“All efforts to predict the best vaccine candidates and fine-tune pandemic control measures hinge on understanding the immune response to the virus,” said Dr Shane Crotty, also a professor in the Center for Infectious Disease and Vaccine Research. “People were really worried that COVID-19 does not induce immunity and reports about people getting re-infected reinforced these concerns, but knowing now that the average person makes a solid immune response should largely put those concerns to rest.”
In an earlier study, Sette and his team used bioinformatics tools to predict which fragments of SARS-CoV-2 are capable of activating human T cells. In their current study, the scientists tested whether the T cells isolated from adults who had recovered from COVID-19 without major problems recognised the predicted protein fragments, or so-called peptides, from the virus itself. The scientists pooled the peptides into two groups:
- The first so-called mega-pool included peptides covering all proteins in the viral genome apart from SARS-CoV-2’s S protein
- The second mega-pool specifically focused on the S protein that dots the surface of the virus, since almost all of the vaccines under development right now target this coronavirus S protein.
“We specifically chose to study people who had a normal disease course and did not require hospitalisation to provide a solid benchmark for what a normal immune response looks like, since the virus can do some very unusual things in some people,” said Sette.
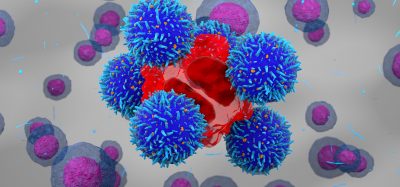
The researchers found that all COVID-19 patients had a solid CD4, or ‘helper’, T-cell response, which aids in antibody production. Almost all patients had produced virus-specific CD8, or ‘killer’, T cells, which eliminate virus-infected cells.
“Our data show that the virus induces what you would expect from a typical, successful antiviral response,” said Crotty.
The researchers emphasise that although these results do not preclude that the immune response to SARS-CoV-2 may be detrimental, they provide an important baseline against which individuals’ immune responses can be compared.
“We have a solid starting foundation to now ask whether there’s a difference in the type of immune response in people who have severe outcomes and require hospitalisation versus people who can recover at home or are even asymptomatic,” added Sette. “Not only that, we now have an important tool to determine whether the immune response in people who have received an experimental vaccine resembles what you would expect to see in a protective immune response to COVID-19, as opposed to an insufficient or detrimental response.”
The teams also investigated the T-cell response in blood samples that had been collected between 2015 and 2018, before SARS-CoV-2 started circulating. Many of these individuals had significant T-cell reactivity against SARS-CoV-2. However, the researchers note that everybody has almost certainly seen at least three of the four common cold coronaviruses, which could explain the observed cross-reactivity.
The researchers say that it is still unclear whether this observed cross-reactivity provides at least some level of pre-existing immunity to SARS-CoV-2 and therefore could explain why some people or geographical locations are hit harder by COVID-19.
“Given the severity of the ongoing COVID-19 pandemic, any degree of cross-reactive coronavirus immunity could have a very substantial impact on the overall course of the pandemic and is a key detail to consider for epidemiologists as they try to scope out how severely COVID-19 will affect communities in the coming months,” said Crotty.
The study was published in Cell.
Related topics
Disease Research, Immunology, Immunotherapy, Research & Development, Vaccine
Related conditions
Coronavirus, Covid-19
Related organisations
La Jolla Institute for Immunology
Related people
Dr Alessandro Sette, Dr Shane Crotty