Macaques and baboons show success as models to study SARS-CoV-2
Posted: 6 January 2021 | Victoria Rees (Drug Target Review) | No comments yet
Researchers have shown rhesus macaques and baboons develop strong signs of acute viral infection from SARS-CoV-2, making them ideal models.


Scientists have published their findings regarding a comprehensive animal model that can be used to study SARS-CoV-2. The research was conducted at Texas Biomedical Research Institute (Texas Biomed) and Southwest National Primate Research Center (SNPRC), US.
The study evaluated three non-human primate (NHP) species (Indian rhesus macaques, African baboons and new-world origin common marmosets) and young and old animals, to determine susceptibility to the SARS-CoV-2 virus and the development of COVID-19 disease.
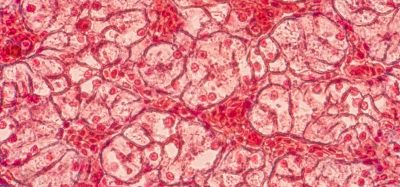
The team of 43 researchers reported clinical, viral, imaging, immunological and histopathological findings during SARS-CoV-2 infection/COVID-19 disease in all three species of NHPs. The study ultimately found that NHPs showed similar progression of SARS-CoV-2 infection to that of humans, with some becoming more ill than others and signs of the virus in both the upper and lower respiratory tracts and signs of pneumonia.
Over the course of the study, the macaque and baboon models showed significant promise as animal models for COVID-19 disease studies moving forward. Based on outcomes, the researchers recommended use of the macaque as a model to help develop vaccines, while the baboon showed greater disease development, making it a potential option for evaluating antiviral therapeutics and co-morbidities, such as understanding the connection between COVID-19 and diabetes or COVID-19 and heart disease.
While previous animal studies showed the macaque to be a viable model for SARS-CoV-2, this was the first time that researchers performed a longitudinal study of three different NHPs and in both young and older macaques to determine if age is a factor in disease progression.
Results showed that the macaque and baboon models develop strong signs of acute viral infection leading to pneumonia and the NHP immune system mounts a strong response and clears the infection. Specialised sets of myeloid cells (phagocytes) move from blood to the lungs and secrete high levels of Type I interferons, cytokines or proteins that send chemical messages required for controlling viruses in general and coronaviruses in particular. The appearance of these specialised phagocytes (cells that ingest foreign particles or dying cells in the body) corresponded with a decline in measurable amounts of virus and disease parameters. The researchers found that the longitudinal study of young and old animals showed little difference. However, the virus appears to persist and shed longer in the baboons and create greater pathology in the lungs. The marmoset model did not show any significant signs of disease progression.
This study was also the first report of SARS-CoV-2 infection specifically altering lymphoid cells in the lung, which generated a strong and very specific immune response in the macaque, enabling the animals to clear the virus. This finding indicates the NHP model will be useful in understanding the immune response to SARS-CoV-2 and aid in the development of interventions that can create a similar response, as well as help evaluate the safety and effectiveness of vaccines, which require a specific immune response in order to be effective.
“Texas Biomed was able to launch and complete the most comprehensive animal model study to date (June 2020) that has provides scientists greater understanding of the immune response to SARS-CoV-2 and definitively identifies two possible animal models to help move vaccines and therapeutics forward,” said Dr Larry Schlesinger, Texas Biomed President and Chief Executive Officer.
“Finding the appropriate animal models for COVID-19 allows for these critical discoveries to happen now and they are an important step in combatting this disease,” said Dr Deepak Kaushal, lead principal investigator on the macaque portion of the study. “Without well-documented animal data, the US Food and Drug Administration (FDA) is unlikely to license a vaccine or antiviral therapy for human use, even those currently undergoing human trials, because animal model data assure us that we have a complete picture of the disease and how humans may respond to potential therapies.”
The findings were published in Nature Microbiology.
Related topics
Disease Research, In Vivo, Proteomics, Research & Development
Related conditions
Covid-19
Related organisations
Southwest National Primate Research Center (SNPRC), Texas Biomedical Research Institute
Related people
Dr Deepak Kaushal, Dr Larry Schlesinger