New drug target for non-small cell lung cancer identified
Posted: 6 January 2021 | Victoria Rees (Drug Target Review) | No comments yet
A new study has suggested that the enzyme GFPT2 could be a useful target for non-small cell lung cancer (NSCLC).
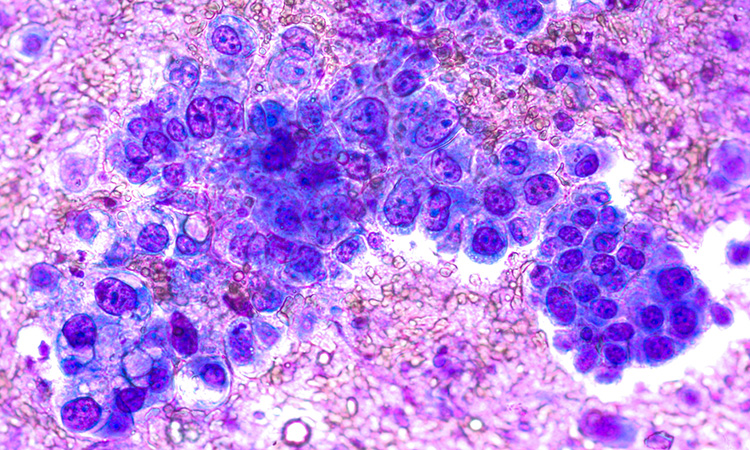
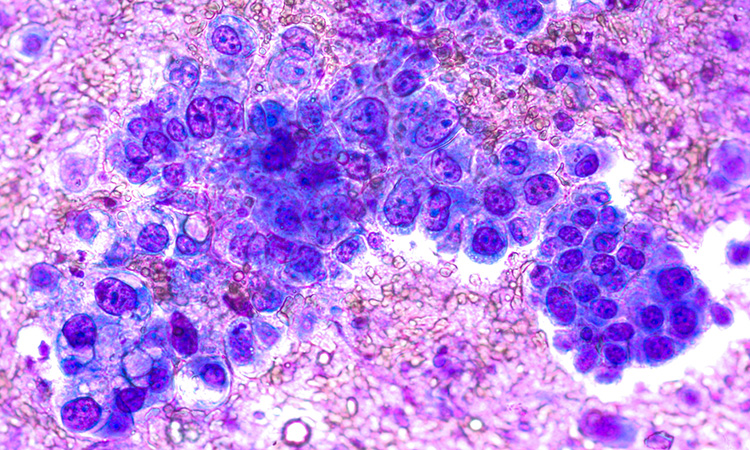
Researchers have discovered a new metabolic vulnerability in a highly aggressive form of non-small cell lung cancer (NSCLC). According to the team, these findings could pave the way for new treatments for patients with mutations in two key genes – KRAS and LKB1. Patients whose tumours contain both of these mutations, known as KL tumours, have poor outcomes and usually do not respond to immunotherapy.
The study on cancer was conducted at the Children’s Medical Center Research Institute (CRI) at the University of Texas (UT) Southwestern, US.
“We used to think that most tumours rely on the same handful of metabolic pathways to grow, but we have learned over the last decade that this is an oversimplification. Instead, different tumour subclasses have particular metabolic needs arising from mutations in key genes. Understanding how specific combinations of mutations promote tumour growth and metastasis may allow us to design tailored therapies for patients,” said Dr Ralph DeBerardinis.
To uncover new metabolic vulnerabilities, the scientists compared metabolic properties of KL tumours genetically engineered in mice to tumours containing different mutations and to the normal lung. They discovered that the hexosamine biosynthesis pathway (HBP) is activated in KL tumours. These findings were consistent with previous research that showed KL cells reprogramme carbon and nitrogen metabolism in ways that promote their growth but increase their sensitivity to particular metabolic inhibitors.
The HBP allows cells to modify proteins through glycosylation, which facilitates protein trafficking and secretion. The high rate of protein production that fuels KL tumour growth is thought to require activation of the HBP. To develop ways to inhibit the HBP, the researchers next identified the enzyme GFPT2 as a key liability in KL tumours. Genetically silencing or chemically inhibiting this enzyme suppressed KL tumour growth in mice, but had little effect on the growth of tumours containing only the KRAS mutation. Altogether, the findings indicate the selective importance of the HBP in KL tumours and suggest that GFPT2 could be a useful target for this aggressive subtype of cancer.
“Since no specific inhibitor against GFPT2 exists, our next step is to see if blocking certain steps in the glycosylation pathway could be therapeutically beneficial. Ultimately we are looking for options that can help stop the growth and spread of these aggressive tumours and cancers,” said Dr Jiyeon Kim, who co-led the study.
The study on non-small cell lung cancer was published in Nature Metabolism.
Related topics
Drug Targets, Enzymes, Oncology, Research & Development, Targets
Related conditions
Non-small cell lung cancer (NSCLC)
Related organisations
Texas University
Related people
Dr Jiyeon Kim, Dr Ralph DeBerardinis.