What we know about COVID-19 and the inflammatory response
Posted: 10 March 2021 | Sadya Arnett (Scientific Writer) | 1 comment
A year on from discovering COVID-19 we are starting to understand why some people suffer more severely after infection. Sadya Arnett discusses recent research into the interconnection between host inflammation and SARS-CoV-2.
Patients that show more difficulty in overcoming COVID-19 include the elderly and people with noncommunicable chronic diseases (NCDs) such as diabetes and cardiovascular disease.1 They are more likely to require intensive care, have lower survival rates and face more chance of developing long term complications.2 It is now recognised that these patients show a more extreme inflammatory response when infected by COVID-19, which is thought to be why they suffer more severely.1
Inflammation is normal in response to injury or pathogenic infection, but it appears that patients with NCDs or the elderly demonstrate pre-heightened inflammatory levels. This can make them subject to uncontrolled inflammation when infected by the coronavirus, leading to a cytokine storm.1 This is an extreme release of cytokines in response to infection due to a loss of regulation on the release of pro-inflammatory cytokines. For example, pro-inflammatory markers associated with a cytokine storm have been detected in diabetic COVID-19 patients.2 Moreover, a cytokine storm is proposed to be the cause of acute respiratory distress syndrome (ARDS) and multiple organ failure,3-4 both of which present in severe COVID-19 cases.
 Observational studies of COVID-19 patients that required intensive care show higher than normal levels of the pro-inflammatory factors IL-2, IL-7, IL-10, granulocyte colony-stimulating factor (G-CSF), IP-10, MCP1, macrophage inflammatory protein 1α (MIP1α) and tumour necrosis factor (TNF)11 in their blood plasma. Clinical observations revealed that IL-6 was higher in non-survivors compared to those that managed to recover.4 Furthermore, high levels of cytokines like TNF are associated with septic shock and multiple organ failure, leading scientists to hypothesise this could also be causing myocardial damage and circulatory failure seen in some COVID-19 patients.4
Observational studies of COVID-19 patients that required intensive care show higher than normal levels of the pro-inflammatory factors IL-2, IL-7, IL-10, granulocyte colony-stimulating factor (G-CSF), IP-10, MCP1, macrophage inflammatory protein 1α (MIP1α) and tumour necrosis factor (TNF)11 in their blood plasma. Clinical observations revealed that IL-6 was higher in non-survivors compared to those that managed to recover.4 Furthermore, high levels of cytokines like TNF are associated with septic shock and multiple organ failure, leading scientists to hypothesise this could also be causing myocardial damage and circulatory failure seen in some COVID-19 patients.4
How does COVID-19 produce inflammation?
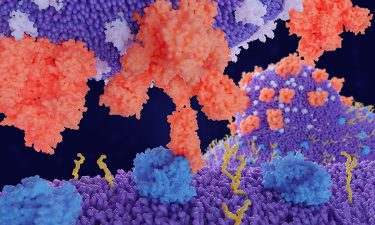
COVID-19 most commonly infects the lower respiratory tract of its host via attachment of the virus’ Spike (S) protein to the human Angiotensin-converting enzyme (ACE2) receptors found on the alveolar epithelial cells.1 ACE2 receptors are also present on capillary endothelial cells meaning organs rich in these cells are vulnerable to secondary infection from SARS-CoV-2 including the kidney, gut and brain.5 The S protein must be cleaved using host proteases such as transmembrane protease serine protease (TMPRSS2). This allows for the viral and cellular membranes to fuse, enabling the eventual entry of the virus into the host cell.5 ACE2 has a homeostatic function of controlling the deleterious effects of the ACE/RAS pathway through negative feedback. When SARS-CoV-2 is bound to ACE2 receptor the enzyme cannot carry out this regulatory function.
Clinical observations revealed that IL-6 was higher in non-survivors compared to those that managed to recover”
ACE is expressed predominantly on vascular endothelium of the lungs and kidneys and the lung epithelium. It converts Angiotensin I to Angiotensin II (AngII).5 AngII causes the adrenal cortex to release aldosterone causing sodium and water retention but it is also a potent vasoconstrictor which is detrimental to endo- and epithelial function.5 AngII has also been shown to induce the pro-inflammatory cytokines IL-6 and TNFα, inducing an influx of immune cells to the infected site, causing vascular injury.5 Elevated AngII can eventually lead to fibrosis, inflammatory injuries and blood clots.5 Autopsy reports of recent COVID-19 infected individuals showed widespread alveolar damage, capillary congestion and the presence of microthrombi (small clots).5 ACE2 counteracts the effects of ACE by degrading AngII to Ang1-7, thereby preventing vasoconstriction, thrombophilia, micro-thrombosis, alveolar epithelial injury and respiratory failure.5
The AngII mechanism is not the only way COVID-19 can trigger the host’s inflammatory response. Using pattern-recognition receptors (PRRs) the host detects pathogen-associated molecular patterns (PAMPs) from the virus. This causes local inflammation via activation of the MAPK pathway and increased expression of pro-inflammatory factors which attract monocytes and macrophages to infection sites like the lungs.1, 4 Increased levels of pro-inflammatory cytokines and chemokines IL-6, IFNγ, MCP1 and IP-10 enter the bloodstream, attracting T lymphocytes and monocytes to infiltrate the virally infected cells which also creates inflammatory injury.4
Uncontrolled inflammation at the infected lung site will instil alveolar damage such as desquamation of the alveolar cells, hyaline membrane formation (the build-up of dead cells and proteins) and pulmonary oedema (swelling of the lungs due to excess fluid). These physiological changes cause reduced gas exchange leading to difficulty in breathing and low blood oxygen levels with the lungs becoming susceptible to secondary infections like pneumonia4.
Why are NCD and elderly patients more vulnerable?
Clinical observations reveal that people with NCDs express more ACE2, which may be why people in this category are more vulnerable as they have more opportunities for SARS-CoV-2 infection.1 Furthermore, it is recognised that those with NCDs already experience systemic inflammation in the body. These factors may be why these groups of people will have more difficulty recovering from COVID-19.1
Anti-inflammatory treatments
An array of clinical anti-viral drugs are being trialled for their efficacy in hospitalised COVID-19 patients. Some of these antiviral treatments may be successful because of their anti-inflammatory properties. For example, chloroquine (CQ) and hydroxychloroquine (HCQ) are antivirals already used against Hepatitis B, H1N1 and Zika virus. They are also used as anti-inflammatories against autoimmune diseases like rheumatoid arthritis.5
In relation to COVID-19, these drugs disrupt glycosylation and protein maturation of ACE2, preventing the virus attaching to this receptor.6 Their presence also seems to inhibit cytokine production of IL-1, IL-2, IL-6, IL-8 TNFα and IFNγ. Both actions help to manage the host’s inflammatory response, lowering the chances of a cytokine storm.6 Thus CQ and HCQ could be valuable therapies for NCD patients with already elevated inflammatory levels. Chloroquine is currently being used to treat patients in China between the ages of 18 and 65 years old.3
Corticosteroids are a common immunosuppresent5 thus another potential treatment to regulate the uncontrolled inflammatory response seen in COVID-19 patients. Providing the timing of administration is correct, they provide beneficial effects by reducing fever and improving lung oxygenation.3 In a study of Severe Acute Respiratory Syndrome (SARS) patients, corticosteroid use significantly reduced hospital stay, mortality rate and secondary infections rarely took place in those using this treatment. However, timing of drug administration is crucial because patients dosed too early showed increased plasma viral load as the host immune defence was inhibited.3
In a relatively short space of time, scientists have understood the link between COVID-19 and the host’s inflammatory response. This knowledge has led the scientific community to consider re-purposing existing drugs with anti-inflammatory properties as possible treatments to help cure patients with severe COVID-19.
About the author
Sadya Arnett recently graduated from the University of East Anglia (UEA) in biological sciences. She has a keen interest in food, health and animal science disciplines.
References
- Zabetakis I, Lordan R, Norton C & Tsoupras A. COVID-19: The inflammation link and the role of nutrition in potential migration. Nutrients. 19 May 2020. 12 (1466)
- Filardi T & Morano S. COVID-19: is there a link between the course of infection and pharmacological agents in diabetes? Journal of Endocrinological Investigation. 3 June 2020
- Ye Q, Wang B, Mao J. The pathogenesis and treatment of the ‘cytokine storm’ in COVID-19. Journal of Infection. 10 April 2020. 80: 607-613
- Tay M, Poh C, Renia L, MacAry P & Ng L. The trinity of COVID-19: immunity, inflammation and intervention. Nature Reviews Immunology. 28 April 2020. 20: 363-374
- Samavati L. & Uhal B. ACE2, much more than just a receptor for SARS-COV-2. Frontiers in Cellular and Infection Microbiology. 5 June 2020. 10 (317)
- Tufan A, Avanoglu-Guler A, & Matucci-Cerinic M. COVID-19, immune system response, hyperinflammation and repurposing antirheumatic drugs. Turkish Journal of Medical Sciences. 21 April 2020. 50: 620-632
Related topics
Disease Research, Drug Development, Drug Repurposing, Immunology






Thanks for the article! I was curious are there studies or evidence showing that if someone already has chronic inflammation that when they get covid the symptoms tend to be worse?