Scientists discover neuron-like communication in gut cells
Posted: 30 July 2025 | Drug Target Review | No comments yet
Scientists in Singapore have discovered that gut support cells – known as telocytes – use neuron-like extensions to deliver signals directly to intestinal stem cells. This could lead to new treatments for diseases such as inflammatory bowel disease and colon cancer.
Researchers from Duke-NUS Medical School and Nanyang Technological University (NTU) have discovered a surprising communication system within the gut. Support cells known as telocytes use fine extensions – like neurons in the brain – to send signals directly to intestinal stem cells. The findings, published in Developmental Cell, tackle common assumptions about how the gut maintains and repairs itself, which could allow for future treatments for inflammatory bowel disease (IBD) and colon cancer.
Gut stem cells depend on precise instructions
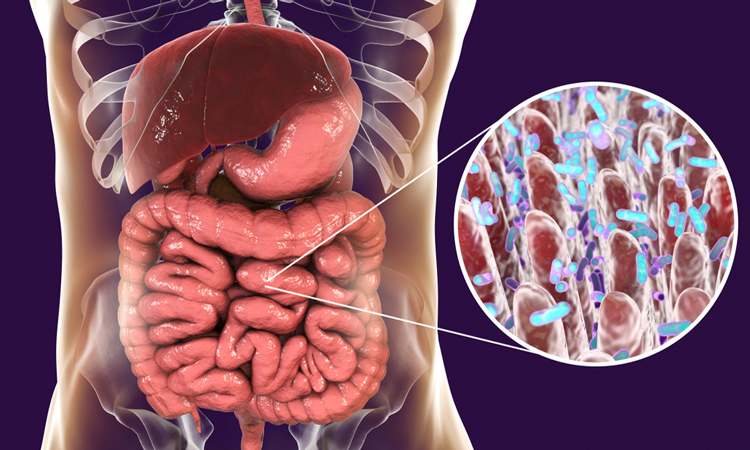
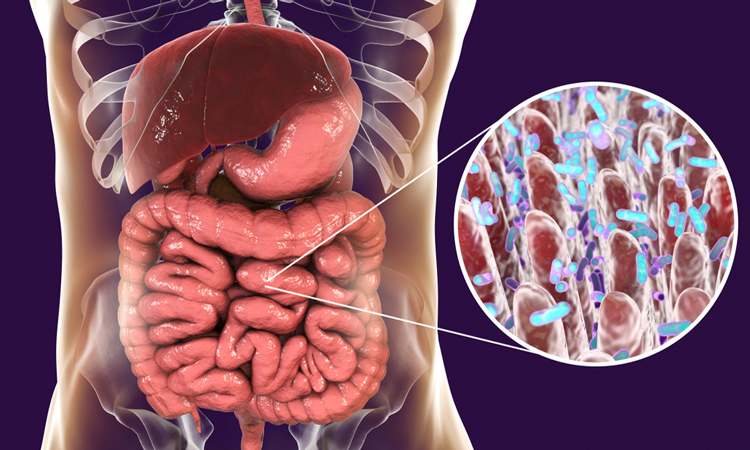
The intestinal lining is one of the most active tissues in the human body, renewing itself every few days. This fast regeneration relies on a small group of stem cells located in tiny pockets in the gut lining called crypts. These stem cells divide and differentiate into various cell types needed for gut function – guided by chemical instructions from surrounding support cells within their niche.
Until now, scientists believed that Wnt signals – key molecules regulating stem cell behaviour – drifted through tissue by diffusion. However, this random process seemed insufficient to explain the timing and accuracy of stem cell control.
“We discovered that these signals aren’t just drifting through tissue. They’re being delivered with surprising precision from the niche to the stem cells by specialised cells, or telocytes – changing the way we think about cellular communication in the gut; similar to how neurons pass signals to one another in the brain,” explained Professor David Virshup, Director of the Programme in Cancer and Stem Cell Biology at Duke-NUS Medical School and co-corresponding author of the study.
Telocytes use neuron-like extensions
Telocytes are special because they extend long, thin projections called cytonemes that reach directly from the telocyte to a specific stem cell. Using high-resolution fluorescence and electron microscopy, the researchers observed that telocytes in mouse intestines use cytonemes to deliver Wnts directly to individual stem cells.
The researchers found that the contact points between telocytes and stem cells closely resemble synapses – the one-to-one connections between nerve cells
The researchers found that the contact points between telocytes and stem cells closely resemble synapses – the one-to-one connections between nerve cells. This targeted delivery system ensures that Wnt molecules reach their intended destination efficiently.
“This kind of direct, cell-to-cell communication highlights a new level of precision in how secreted molecules are delivered to their target cell,” Assistant Professor Alexander Ludwig from NTU Singapore, a co-author of the study, said. “It’s a striking example of how imaging at different scales coupled with new protein tagging approaches can uncover novel mechanisms and change paradigms.”
Proteins behind the system
To explore how this signalling system functions, the team studied the structural proteins essential for cytoneme formation. When two key proteins – KANK and Liprin – were disrupted, the cytonemes failed to form or function, and Wnt delivery broke down.
“Sometimes when you study the basics closely, you uncover something transformative. This system of targeted signalling was hiding in plain sight, and now that we see it, it reshapes our understanding of the biology of stem cells in the gut,” Principal Research Scientist Dr Gediminas Greicius, first author of the study, said.
Implications for disease and regenerative medicine
Although the research focused on healthy tissue, the implications are vast. Disrupted Wnt signalling is linked to colon cancer, while impaired signalling may contribute to chronic IBD conditions such as Crohn’s disease and ulcerative colitis , which are increasingly common across the world.
“This discovery could change how we approach tissue repair and regenerative medicine,” said Professor Patrick Tan, Senior Vice-Dean for Research at Duke-NUS. “If we can harness or restore this precise mode of signalling, it may enhance the effectiveness of stem cell therapies and help develop more targeted treatments for gut-related diseases. It’s a strong example of how basic science drives real-world impact.”
Related topics
Analysis, Cancer research, Cell Regeneration, Disease Research, Imaging, Regenerative Medicine, Stem Cells
Related conditions
Cancer, Colon cancer, Inflammatory bowel disease (IBD)
Related organisations
Duke-NUS Medical School, Nanyang Technological University (NTU)
Related people
Alexander Ludwig (Assistant Professor at NTU Singapore), Dr Gediminas Greicius (Principal Research Scientist at Duke-NUS Medical School), Professor David Virshup (Director of the Programme in Cancer and Stem Cell Biology at Duke-NUS Medical School), Professor Patrick Tan (Senior Vice-Dean for Research at Duke-NUS)