Potential sepsis prevention in burn patients found with novel approach
Posted: 4 September 2019 | Rachael Harper (Drug Target Review) | No comments yet
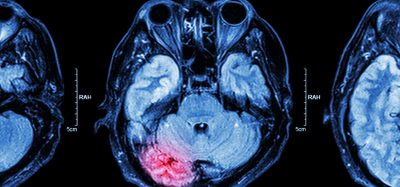
A new study has demonstrated the possibility of treating antibiotic-resistant Pseudomonas aeruginosa which causes sepsis in burn patients.


TTUHSC graduate student Taylor Lenzmeier (left) and Abdul Hamood, PhD, from the Texas Tech University Health Sciences Center School of Medicine, collaborated with others to investigate the feasibility of developing a topical treatment unrelated to conventional antibiotics that can be used to battle Pseudomonas aeruginosa (credit: TTUHSC).
Researchers have investigated the feasibility of developing a topical treatment unrelated to conventional antibiotics that can be used to battle Pseudomonas aeruginosa, a pathogen that causes sepsis in burn patients.
The research by Abdul Hamood, PhD, a professor for the Department of Immunology and Molecular Microbiology at the Texas Tech University Health Sciences Center (TTUHSC) School of Medicine and a team of collaborators used probiotic bacteria and its superior by-products to prevent Pseudomonas infection. This is because Pseudomonas aeruginosa has developed resistance to antibiotics.
“It’s almost this idea of using probiotics as an alternative to antibiotics,” explained Taylor Lenzmeier, a TTUHSC graduate student and the study’s lead author.
Automation now plays a central role in discovery. From self-driving laboratories to real-time bioprocessing
This report explores how data-driven systems improve reproducibility, speed decisions and make scale achievable across research and development.
Inside the report:
- Advance discovery through miniaturised, high-throughput and animal-free systems
- Integrate AI, robotics and analytics to speed decision-making
- Streamline cell therapy and bioprocess QC for scale and compliance
- And more!
This report unlocks perspectives that show how automation is changing the scale and quality of discovery. The result is faster insight, stronger data and better science – access your free copy today
To accomplish this, the Hamood team examined the effectiveness of using a highly concentrated supernatant, or secreted liquid by-product, obtained from Lactobacillus gasseri strain 63 AM (LgCS). This supernatant is separated from the LgCS, concentrated and applied to the wound.
The research team found that applying LgCS secretions to the wound inhibited Pseudomonas aeruginosa growth, prevented biofilm development and eliminated any partially developed biofilm.
The study also showed that a single injection of LgCS secretions administered after thermal injury and Pseudomonas aeruginosa infection reduced mortality to zero percent and prevented sepsis in mice. A second injection administered 24 hours later eliminated Pseudomonas aeruginosa from the wound.
Furthermore, using another model of wound infection that does not involve thermal injury, the investigators discovered that treating an infected wound using either LgCS or ceftazidime significantly reduced the mortality rate in mice and treating the infected wound using a combination of LgCS and ceftazidime eliminated mortality in mice. Ceftazidime is an antibiotic used to treat meningitis and several other infections.
Hamood said the next step is to characterise the inhibitory factor that seems to produce such promising results. “Right now, it’s just a crude product and we proved that this crude product is very special,” Hamood said.
There’s a phenomenon occurring, but now we need to discuss and describe what’s causing it and even further, describe the mechanism of action to that wound.”
The study was published in the Journal of Medical Microbiology.
Related topics
Antibiotics, Drug Development, Drug Discovery, Drug Targets, Formulation, Hit-to-Lead, Research & Development
Related conditions
Sepsis
Related organisations
Journal of Medical Microbiology, Texas Tech University Health Sciences Center (TTUHSC) School of Medicine
Related people
Abdul Hamood PhD, Taylor Lenzmeier