Novel siRNA therapy improves psoriasis in mice
Posted: 19 October 2020 | Hannah Balfour (Drug Target Review) | No comments yet
Topical delivery of a small interfering RNA (siRNA) using an ionic liquid complex significantly reduced levels of inflammatory cytokines and symptoms of psoriasis.
To overcome some of the limitations of current psoriasis therapies, researchers have developed an ionic liquid (IL) combination to deliver a small interfering RNA (siRNA)-based treatment directly to the skin. In experiments with murine models of psoriasis, the NFKBIZ siRNA-based treatment significantly reduced levels of inflammatory cytokines and symptoms of psoriasis without systemic side effects.
Psoriasis is a chronic skin condition that causes itchy, red, scaly patches and afflicts more than 125 million people worldwide. Small molecule-based drugs like steroids, can penetrate the skin to treat the condition, but they often cause skin irritation and thinning, their efficacy can also decrease over time. Antibodies that target specific inflammation-related molecules associated with psoriasis have been developed, but because they cannot be delivered topically, they are injected using needles and syringes, which limits their acceptance and can have negative systemic side effects.
A team of researchers at Harvard’s Wyss Institute for Biologically Inspired Engineering and John A. Paulson School of Engineering and Applied Sciences (SEAS), both US, sought to overcome these limitations in their research was published in Science Advances.
“Compared to other technologies that have demonstrated delivery of nucleic acids to the skin, our IL platform offers unique opportunities in terms of tunability, an excellent safety profile, and economical scale-up,” said first author Dr Abhirup Mandal, a former Postdoctoral Fellow at the Wyss Institute and SEAS who is now a Senior Research Scientist at CAGE Bio. “We think that effective topical delivery of macromolecules will revolutionize the treatment options for debilitating dermatological disorders like psoriasis.”
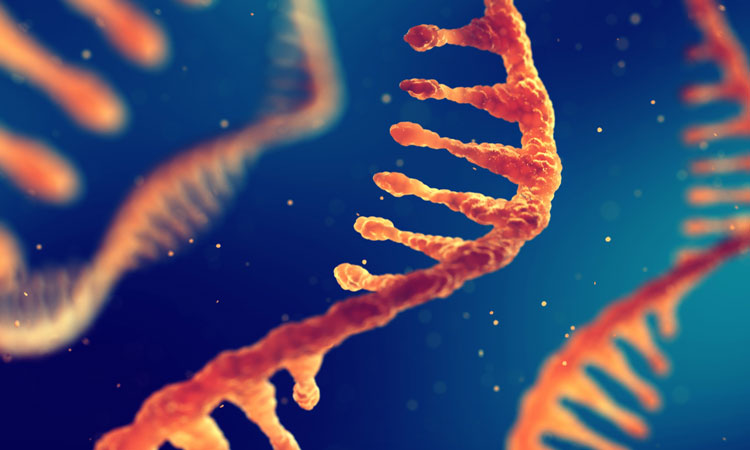
Synthetic siRNAs are non-coding double-stranded RNA molecules that can silence a target gene by destroying its RNA transcripts. This ability makes them very attractive candidates for treating diseases and disorders without modifying the DNA in a patient’s cells. But their potential in medicine has so far been curtailed due to their structure: siRNAs are large, hydrophilic molecules and therefore have a hard time crossing hydrophobic cellular membranes.
To overcome this, the team hypothesised that the ILs they had recently discovered, which are essentially salts that are liquid at room temperature, may be able to stabilise siRNAs and improve their penetration across lipid-based cell membranes, enabling localised gene silencing.
The team first created a library of different ILs, then tested combinations of them to see which had the physical and chemical properties they were looking for. They settled on a mixture of CAGE (choline and geranic acid) and CAPA (choline and phenylpropanoic acid) that helped associated siRNA molecules retain their structural integrity and led to increased siRNA penetration into pig skin in vitro. When they applied the CAGE+CAPA mixture as a thick topical liquid to the skin of living mice, they observed no inflammation or irritation, indicating that it was non-toxic.
Armed with their delivery vehicle, the team coupled an siRNA designed to silence the NFKBIZ gene, which has been implicated in the upregulation of several inflammatory molecules involved in psoriasis. They applied the IL-siRNA complex to the skin of mice with a psoriasis-like condition for four days, then compared those mice to others that had received CAGE+CAPA with a control siRNA, CAGE+CAPA alone or no treatment.
The mice that were given the NFKBIZ siRNA treatment had reduced epidermal thickening, skin discoloration and keratin overgrowth compared to the other experimental groups, as well as less redness and scaling. They also displayed a significant reduction in the expression of NFKBIZ and other psoriasis-related gene products in their skin cells, demonstrating that IL-siRNA complexes can induce a therapeutic effect by silencing a target gene in vivo following topical administration.
“Topical creams have been used to treat skin conditions for hundreds of years, but the skin is a very effective barrier against most substances, which limits their effectiveness. Being able to bridge that barrier to deliver nucleic acid therapeutics directly to skin cells is a huge accomplishment in the quest for targeted, effective therapeutics,” said corresponding author Dr Samir Mitragotri, a Core Faculty member at the Wyss Institute and the Hiller Professor of Bioengineering and Hansjörg Wyss Professor of Biologically Inspired Engineering at SEAS.
According to the team, their IL-based delivery platform can be easily scaled up and tuned to interface with a variety of therapeutic molecules, including DNA and antibodies. It could also allow transdermal drug delivery for the treatment of other dermatologic skin conditions including eczema.
Moving forward, Mitragotri’s lab is initiating new collaborations with researchers focused on understanding local and systemic mechanisms associated with autoimmune and inflammatory diseases in the skin.
Related topics
Drug Delivery, Drug Development, Drug Targets, Genomics, Immunology, In Vivo, RNAs, Therapeutics
Related conditions
Psoriasis
Related organisations
John A. Paulson School of Engineering and Applied Sciences (SEAS), Wyss Institute for Biologically Inspired Engineering
Related people
Dr Abhirup Mandal, Dr Samir Mitragotri