Rebalancing the immune system to treat autoimmune disease
Posted: 2 March 2020 | Hannah Balfour (Drug Target Review) | No comments yet
Dr Nicolas Poirier reveals how immunotherapies can be designed to recalibrate the immune system for long-term maintenance of autoimmune remission.


Autoimmune conditions affect more than 23.5 million Americans and as many as one in four in the UK. According to recent statistics these conditions are on the rise and some, including Type I diabetes, are three times more common that a few decades ago. While treatments have been developed, there is no cure for autoimmune conditions – most therapeutics focus on relieving inflammation and the pain associated with it.
Drug Target Review’s Hannah Balfour spoke with Dr Nicolas Poirier, the Chief Scientific Officer (CSO) of OSE Immunotherapeutics, to understand their novel approach to targeting and treating autoimmune diseases; using immunology to rebalance the immune system.
…because their therapeutics target the immune system, rather than a localised specific tissue, the products are transferable between different autoimmune conditions”
“A lot of companies focus on inhibiting or killing immune cells, but what we have learned in the last five to 10 years is that not all immune cells are pathogenic. There are ‘bad guys’ of course, but there are also ‘good guys’ in the immune system, which help to fight or control autoimmune attacks,” explained Dr Poirier. He clarified that for each immune cell, there is a corresponding regulatory subtype, such as the well-known T regulatory (Treg) cells. B cells also have a regulatory subtype and so do macrophages.
Dr Poirier’s team target their products to specifically inhibit the pathogenic cells and activate the regulatory cells, manipulating the balance of the immune system to reduce autoimmunity. While this may have various short-term effects on disease symptoms, the overarching goal is to maintain remission and prevent flare-ups in the long term.
Current OSE immunotherapies
At present, the company has two therapeutics in trials, which, according to their CSO, have similar effects but utilise different biologic mechanisms of action.
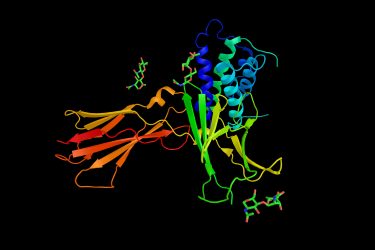
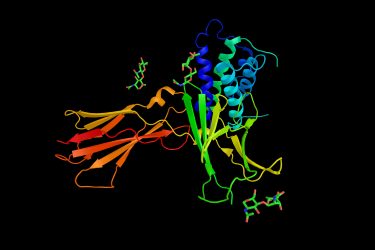
Both are therapies using monoclonal antibody (mAb) fragments as their active pharmaceutical ingredient (API). Dr Poirier revealed the use of fragments was particularly important in establishing a safe level of toxicity.
OSE-104 is a mAb fragment therapy which selectively binds to the CD28 T-cell receptor to block activation of T cells that have the potential to be pathogenic. They also discovered that their fragment can promote Treg cell expansion.According to Dr Poirier, other companies have attempted to develop similar therapies using full mAbs and despite working well in a murine model, “they turned out to be traumatically toxic in humans, because they activate the receptors and as a result the whole immune system.” Instead, his team developed antibody fragments large enough to specifically bind target receptors, but that are unable to activate the receptors they bind to, blocking them instead.
Interleukin 7 (IL-7) is a haematopoietic growth factor secreted by stromal cells in the bone marrow and thymus. It is produced by keratinocytes, neurons and epithelial cells, but is not by normal T lymphocytes.
It is also thought that CD127 may be involved in transforming T cells into memory T lymphocytes.A second drug, OSE-127, with a similar mode of action, is expected to enter Phase II trials in 2020. These immunomodulatory mAb fragments target the CD127 receptors on the surface of T cells. CD127 receptors are alpha chains of IL-7 receptors (IL-1Rs) that bind IL-7 and are expressed on the surface of effector T cells. IL-7 regulates the migration of effector T lymphocytes, particularly in the gut. Therefore, the blockade of IL-7R prevents pathogenic T cells from entering gut tissue to cause inflammatory bowel disease (IBD).
Memory T cells circulate for years after an initial infection and prompt faster future responses to their specific antigens. According to Dr Poirier, the production of memory T cells against autoantigens is responsible for the chronicity of autoimmune conditions such as IBD, because “each time we have an expansion of memory T cells which recognise autoantigens, we have a relapse of the disease.”
Dr Poirier also added that OSE-127 has a further action; IL-7 signalling effects transcription, promoting the proliferation and survival of T cells. By blocking this action, OSE-127 prevents the long-term survival of immune cells such as memory T cells.
Research challenges
Dr Poirier explained that the main challenges in the field of autoimmune therapy research are obtaining and using models that accurately reflect the human condition and immune system.


He revealed: “one of most challenging aspects of targeting the immune system is the translation from technical research which is based on in vitro assays on human cells and in vivo in mice to then a therapeutic in a human patient.”
According to Dr Poirier, they are now involved in a human translational immunology programme to overcome the inaccuracies of animal models. Within this programme they are moving away from the use of animal models and instead are developing ex vivo tissue sample assays from patients. As part of the project, they have access to samples, such as skin from psoriasis patients or colon tissue from IBD patients, on which they can directly test drug candidates on the pathogenic tissue that contains both the pathogenic and regulatory immune cells. “Using this we can directly demonstrate or identify if the drugs work exactly as we want.”
Moving forward
Dr Poirier also revealed that these therapies are still proof-of-concept, from which they intend to learn and optimise their system. Due to their therapeutics targeting the immune system, rather than a localised specific tissue, the products are transferable between different autoimmune conditions. As a result, he suggested that the time spent modifying and developing these pharmaceuticals to be as efficacious and targeted as possible, will make future developments less costly because they can continue to modify and extend the indications. A further area of discovery Dr Poirier believes will be important in the future is working on actively resolving inflammation in autoimmune conditions.
Conclusion
Dr Poirier presents a novel approach for the treatment of autoimmune conditions, moving away from past techniques of broad immunosuppression and towards selectively activating and repressing different subtypes of immune cells. Moving forward, Dr Poirier suggests there will be further modification and development of their mAb fragments in order to target other immune cells related to different conditions.
He also highlighted that progression in R&D models, such as ex vivo patient tissue samples, should also contribute to future success and drug discovery.
Related topics
Antibodies, Biologics, Biopharmaceuticals, Disease Research, Drug Development, Drug Discovery Processes, Drug Targets, Monoclonal Antibody, Research & Development, T cells, Therapeutics
Related conditions
autoimmune diseases, Inflammatory bowel disease (IBD), type 1 diabetes
Related organisations
OSE Immunotherapeutics
Related people
Dr Nicolas Poirier