A novel CAR T-cell therapy for type 1 diabetes
Posted: 4 December 2020 | Hannah Balfour (Drug Target Review) | No comments yet
Researchers show how genetically engineered five-module chimeric antigen receptor (5MCAR) T cells can be directed to destroy T cells causing autoimmune diseases.
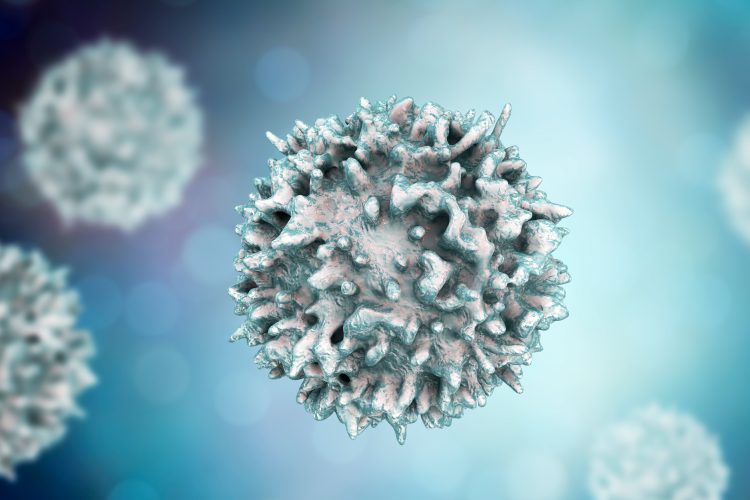
A novel engineered T cell was able to target and destroy the pathogenic autoimmune CD4+ T cell that cause type 1 diabetes in mice. The researchers suggest that their five-module chimeric antigen receptor (5MCAR) T cell could lead to new immunotherapy treatments.
T cells are part of the adaptive immune response, they are activated when their receptors interact with specific antigens presented to them by major histocompatibility complex (MHC) molecules on antigen presenting cells. Killer T cells are the type that work to destroy bacteria, viruses and other pathogens, these cells are activated by a five module domain comprising the T-cell receptor associated with three signalling modules (CD3γε, δε, and ζζ) and a coreceptor module (either CD8 or CD4).
In a new study, Dr Michael Kuhns, an associate professor in the University of Arizona (UArizona) College of Medicine – Tucson Department of Immunobiology, US, and his team of researchers copied the design and created a five-module chimeric antigen receptor (5MCAR) T cell that they then directed to target the autoimmune T cells that mediate type 1 diabetes.
According to Dr Kuhns, their study was an attempt to “build something by biomimicry” and by creating a killer T cell that can recognised another T cell, the team “flipped T cell-mediated immunity on its head.”
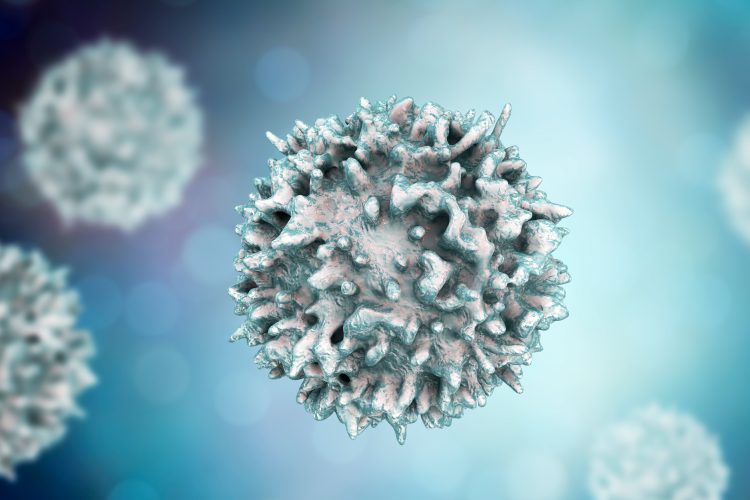
In the study, the UArizona team collaborated with Dr Thomas Serwold of the Harvard Medical School-affiliated Joslin Diabetes Center, to test the 5MCAR T cells in a non-obese diabetic mouse model with promising results. The findings were published in the PNAS.
“When we saw that the 5MCAR T cells completely eliminated the harmful T cells that invaded the pancreas, we were blown away,” Dr Serwold said. “It was like they hunted them down. That ability is why we think that 5MCAR T cells have tremendous potential for treating diseases like type 1 diabetes.”
According to the researchers, the US Food and Drug Administration (FDA) has, so far, approved two chimeric antigen receptor (CAR) T-cell therapies for specific cancers: one for the treatment of children with acute lymphoblastic leukaemia and the other for adults with advanced lymphomas. However, the engineering of those CAR T cells was solely focused on the receptor and did not take into account the function of the surrounding signalling modules or coreceptor.
Dr Kuhns believes that by mimicking the form and function of a natural T cell, including its complex five-module structure, researchers will be able to more specifically target antigens with greater sensitivity in the future, essentially creating a type of personalised immunotherapy.
“I am generally of the belief that evolution converges on related principles to execute related tasks,” Dr Kuhns said. “Basic research from labs around the world, including ours, has helped us to understand the complex structure and function of the five-module molecular machines that have evolved to drive T-cell responses. We think these results show that a biomimetic approach holds promise for CAR engineering.”
Dr Kuhns and Dr Serwold recently received a bridge grant from the National Institute of Allergy and Infectious Diseases (NAID), US, to continue their research into using 5MCAR T cells to prevent autoimmune disease.
“There are many things we do not yet know about this technology,” Dr Kuhns said. “What we know is that it works and it can be very effective in a mouse model of Type 1 diabetes, so that is great. Now, we have a lot more work to do.”
Related topics
Biologics, Chimeric Antigen Receptors (CARs), Drug Development, Drug Leads, Drug Targets, Immunology, Immunotherapy, In Vivo, Therapeutics
Related conditions
autoimmune diseases, type 1 diabetes
Related organisations
Joslin Diabetes Center, University of Arizona (UArizona) College of Medicine, US Food and Drug Administration (FDA)
Related people
Dr Michael Kuhns, Dr Thomas Serwold