Melatonin could act as barrier against SARS-CoV-2 infection
Posted: 28 January 2021 | Victoria Rees (Drug Target Review) | No comments yet
Researchers have suggested using melatonin in a nasal spray to create a protective barrier against SARS-CoV-2 in pre-symptomatic patients.
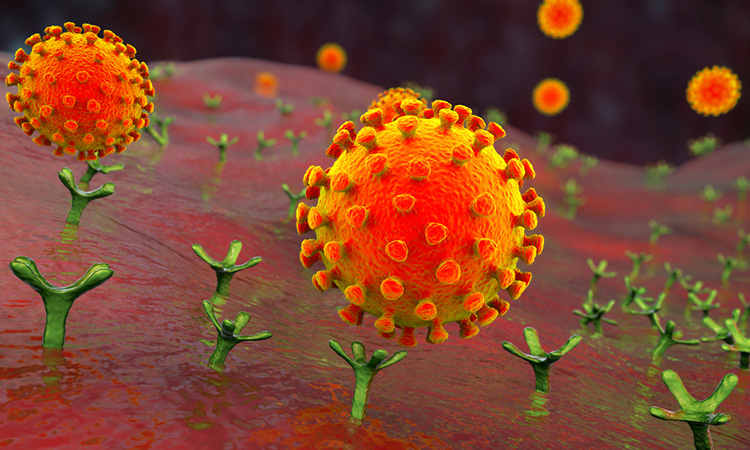
According to a new study, melatonin synthesised in the lungs could act as a barrier against SARS-CoV-2, preventing expression of genes that encode proteins in cells such as resident macrophages in the nose and pulmonary alveoli and epithelial cells lining the alveoli, all of which are entry points for the virus. The hormone, therefore, would prevent infection of these cells by the virus and inhibit the immune response so that SARS-CoV-2 remains in the respiratory tract for a few days, eventually leaving to find another host.
The discovery by researchers at the University of São Paulo (USP), Brazil, offers the prospect of nasal administration of melatonin, in drops or as a spray, to prevent the disease from developing in pre-symptomatic patients.
“We showed that melatonin produced in the lung acts as a barrier against SARS-CoV-2, preventing the virus from entering the epithelium, activating the immune system and triggering the production of antibodies,” said Professor Regina Pekelmann Markus, principal investigator for the project. “This action mechanism by pulmonary melatonin must also involve other respiratory viruses such as influenza.”
Previous research from the team showed that in rodents, the hormone, produced at night by the pineal gland in the brain, can be produced in other organs, such as the lungs. In another study also involving rodents, the researchers showed that resident macrophages in the pulmonary airspace absorb (phagocytise) particles of pollution. This aggressive stimulus induces the production of melatonin and other molecules by the macrophages, engulfing the particulate matter in the air breathed in by the animals and stimulating mucous formation, coughing and expectoration to expel the particles from the respiratory tract. When they blocked melatonin synthesis by resident macrophages, the researchers observed that the particles entered the bloodstream and spread throughout the organism, even invading the brain.
The team decided to investigate whether the hormone performed the same function with regard to SARS-CoV-2. “If so, the virus would not be able to bind to the angiotensin-converting enzyme 2 (ACE2) receptor on cells, enter the epithelium and infect the organism,” Markus said.
To test this hypothesis, the researchers analysed 455 genes associated in the literature with COVID-19 comorbidities, interaction between SARS-CoV-2 and human proteins and viral entry points. The genes had been identified in several studies.
From this group of genes, they selected 212 genes involved in viral cell entry, intracellular traffic, mitochondrial activity and transcription and post-translation processes, to create a physiological signature of COVID-19.
Using RNA sequencing data from a public database, the researchers quantified the level of expression of the 212 COVID-19 signature genes in 288 samples from healthy human lungs.
They then correlated these gene expression levels with a gene index that estimated the capacity of the lungs to synthesise melatonin (MEL-Index) based on their analysis of the lungs in healthy rodents. They found that the lower the index the higher the level of expression of genes that encode proteins for resident macrophages and epithelial cells.
The index also correlated negatively with genes that modify proteins in cell receptor CD147, a viral entry point in macrophages and other immune cells, indicating that normal lung melatonin production may be a natural protector against the virus.
“We found that when MEL-Index was high the entry points for the virus in the lungs were closed and when it was low these ‘doors’ were open. When the doors are shut, the virus wanders around for a time in the pulmonary airspace and then tries to escape in search of another host,” Markus said.
As lung melatonin inhibits transcription of these genes that encode proteins for viral entry point cells, the team say that the application of melatonin directly into the lungs in the form of drops or spray could block the virus.
The study was published in Melatonin Research.
Related topics
Drug Targets, Hormones, Target Molecule, Targets, Therapeutics
Related conditions
Covid-19
Related organisations
University of São Paulo (USP)
Related people
Professor Regina Pekelmann Markus