Could downregulating the Drp1 protein prevent Alzheimer’s progression?
Posted: 4 February 2021 | Hannah Balfour (Drug Target Review) | No comments yet
In this article, we explore the findings of a study that suggests a newly identified pathway, the Drp1-HK1-NLRP3 signalling axis, could be a promising target for therapies to prevent Alzheimer’s disease progression.


Researchers have uncovered a novel signalling pathway that may indicate part of the early stages of Alzheimer’s disease (AD) before the disease progresses to the point where the neuronal loss is too great to reverse. The hope is that by intervening at an earlier stage in the development of AD, scientists may be able to develop treatments to prevent disease progression.
“Only a very small number of medications have been approved for AD since its discovery in 1907. While these medicines augment neurotransmission to provide temporary symptomatic benefit, they do nothing to slow disease progression,” said Andrew Pieper, the Morley-Mather Chair in Neuropsychiatry in the Case Western Reserve University School of Medicine and Director of the Harrington Discovery Institute Neurotherapeutics Center at University Hospitals, US. “Identification of earlier approaches to treating AD… is critical for society as the magnitude of AD is growing explosively with our ageing population.”
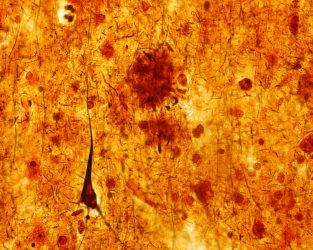
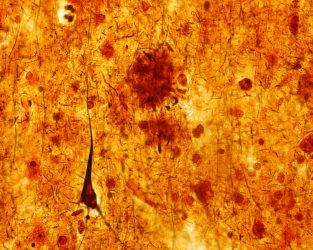
Light micrograph of Alzheimer’s pathology – an Aβ plaque (mid brown circle) and a pyramidal neuron with a neurofibrillary tangle (dark brown structure). The sample is stained with a silver impregnation.
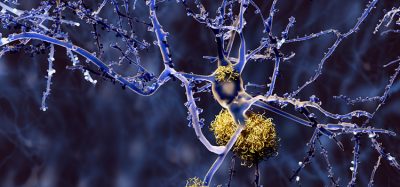
Alzheimer’s is the most common form of dementia (loss of cognitive function), accounting for up to 80 percent of cases. It is a neurodegenerative condition characterised by extracellular senile plaques composed of amyloid-β (Aβ) and intracellular neurofibrillary tangles (NFTs) of hyperphosphorylated tau protein. While these hallmarks of AD are well studied, researchers are yet to discover what the early stages look like and what initiates the disease. The failure of various treatments targeting Aβ and tau in clinical trials is forcing scientists to take a different approach; identifying targets at an earlier stage in the onset of AD that could enable the development of transformative therapies.
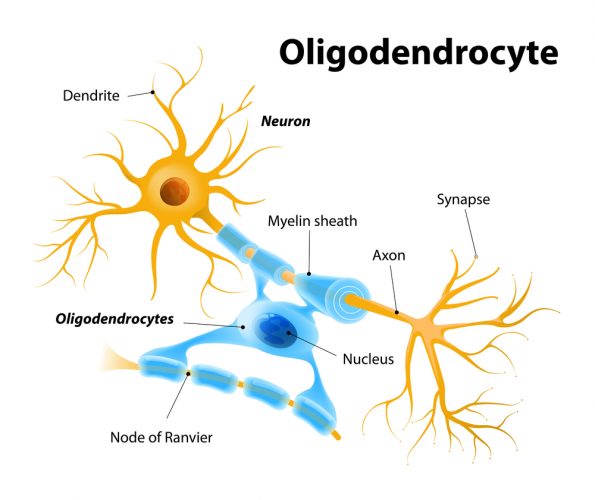
Studies have shown that before Aβ plaques and NFTs become evident, AD patients experience white matter loss and demyelination of their neurons. This is thought to be caused by damage to oligodendrocytes, the cells that produce myelin, which are also known to reduce in number in both AD patients and animal models of AD. Researchers have hypothesised that oligodendrocyte impairment and white matter loss may therefore be the primary events in AD pathology.
But what causes oligodendrocytes to become dysfunctional?
In a new study published in Science Advances, Pieper and colleagues sought to answer this question by investigating the dynamin-related protein 1 (Drp1).
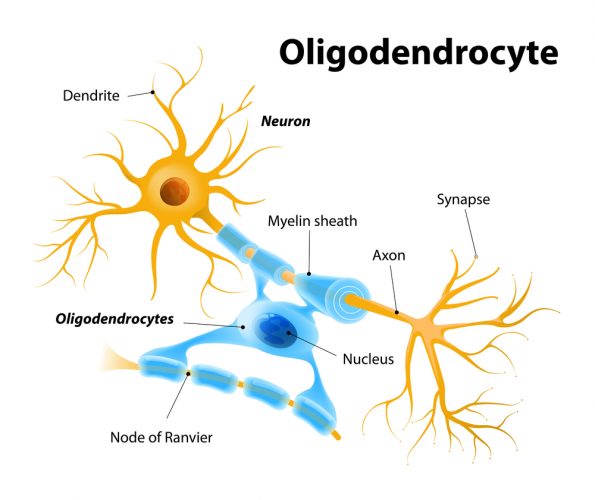
Drp1 controls mitochondrial fission, the process by which mitochondria divide, and is known to have heightened expression in the brains of AD patients and AD mice, as well as in neurons exposed to Aβ peptides in vitro. Mitochondria are the powerhouses of the cell, responsible for much of the metabolism that results in energy production. It is thought that this hyperexpression of Drp1 causes excessive mitochondrial fission, generating reactive oxygen species that proceed to disrupt the production of energy and ultimately cause cells to die. In addition, mature oligodendrocytes are known to rely heavily on glycolysis for their energy supply to perform myelination tasks. Glycolysis occurs outside the mitochondria but provides pyruvate, a product needed for respiration within the mitochondria. As a result, the researchers hypothesised that Drd1 may be hyperactivated in oligodendrocytes, which disrupts glycolysis and may play a role in white matter degeneration.
Findings of the study
In the study, the investigators observed that mature oligodendrocytes from both human AD patients and AD mice had inflammatory injuries associated with the NLR family pyrin domain containing 3 (NLRP3) inflammasome, concomitant with demyelination and axonal degeneration.
The NLRP3 inflammasome is crucial for a long-term inflammatory response. When cells are exposed to stress, the three parts of the inflammasome – NLRP3, an adaptor protein and pro-caspase-1 – assemble intracellularly. This increases the cleavage and activity of caspase-1, which drives Gasdermin D (GSDMD)–mediated pyroptosis, a type of programmed cell death. The increased activity of caspase-1 also causes the downstream release of interleukin-1β (IL-1β), which stimulates downstream cytokines and chemokine receptors to trigger inflammatory responses.
It has been established that the NLRP3 inflammasome can be activated by components of glycolysis and reactive oxygen species, as well as metabolic stress. Researchers have also demonstrated that the NLRP3 inflammasome drives the formation of amyloid plaques and NFTs.
Our results show promise that targeting the Drp1-HK1-NLRP3 pathway and reducing the expression of the Drp1 protein could help reduce the downstream cascade of abnormal brain functions associated with the progression of AD”
In experiments, the researchers observed that downregulating the activity of Drp1 proteins of oligodendrocytes in both cell cultures and transgenic AD mice abolished NLRP3 inflammasome activation and the resulting inflammatory response. The authors highlighted that heterozygous knockout of Drp1 in mature oligodendrocytes of AD mice corrected myelin loss, reduced axonal degeneration and improved cognitive performance.
The researchers also showed that Drp1 hyperactivation in mature oligodendrocytes suppresses glycolysis by inhibiting the hexokinase 1 (HK1) enzyme that initiates it. This inhibition results in metabolic stress that then activates the NLRP3 inflammasome. The resultant inflammatory injury causes the demyelination, white matter degeneration and cognitive impairment in models of AD.
Conclusions
In summary, the team found that Drp1 hyperactivation induces HK1-dependent glycolytic stress, which then elicits NLRP3 activation in mature oligodendrocytes. The result is inflammation, tissue damage and the subsequent loss of white matter and axonal degeneration.
The study’s lead researcher, Xin Qi, a professor in the Department of Physiology and Biophysics at the Case Western Reserve University School of Medicine, said: “This is a missing part of the puzzle. We have discovered a pathway that is accessible to detection and potential treatment, prior to much of the disease’s damage and well before clinical symptoms appear.”
The presence and importance of the Drp1-HK1-NLRP3 signalling axis was confirmed when heterozygous knockout of Drp1 successfully reduced NLRP3 inflammasome activation, attenuated the loss of myelin and axons and improved cognitive performance in mice.
The team summarised that a glycolytic deficiency in oligodendrocytes plays a causal role in AD onset and that the Drp1-HK1-NLRP3 signalling axis could be a key target for therapeutic intervention during the early (white matter degeneration) stage of AD.
Qi concluded: “Our results show promise that targeting the Drp1-HK1-NLRP3 pathway and reducing the expression of the Drp1 protein could help reduce the downstream cascade of abnormal brain functions associated with the progression of AD.” If therapies targeting this pathway can slow, stop or even reverse early-stage AD progression, it may be possible to reduce or delay later stage damage and impairments.
Related topics
Disease Research, Drug Targets, In Vitro, In Vivo, Neurosciences, Protein, Proteomics
Related conditions
Alzheimer's disease (AD)
Related organisations
Case Western Reserve University School of Medicine, Harrington Discovery Institute Neurotherapeutics Center
Related people
Andrew Pieper, Xin Qi