New protocol for intestinal organoid generation developed
Posted: 13 January 2020 | Hannah Balfour (Drug Target Review) | No comments yet
A new process for producing organoids allows researchers to explore intestinal epithelium in isolation and could allow for the development of improved targeted treatments of diseases.
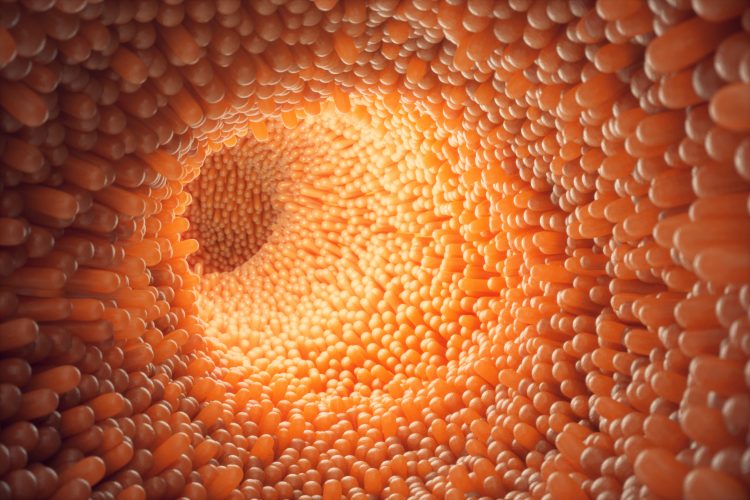
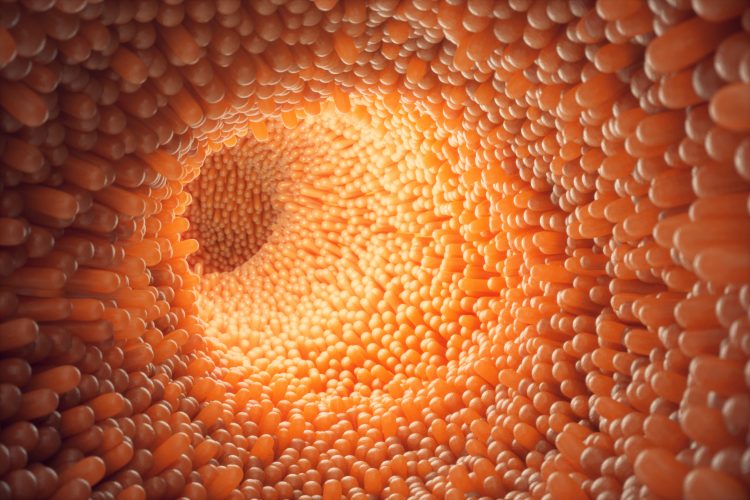
Researchers have created a new protocol for intestinal organoid formation using human induced pluripotent stem cells (hiPSCs). The new technique allows for intestinal epithelial cell response to drug treatment to be studied in isolation and could form the basis of disease research in inflammatory bowel disease, colon cancer and cystic fibrosis.
The study, published in Nature Communications, details how hiPSCs were given growth factor specific to intestinal cells and supported by a gel to create intestine organoids. In other organoid growing protocols, this type of organoid has to be supported by mesenchyme; however, by removing this the researchers were able to study how the epithelial cells of the intestine alone responds to medication.
Researchers at the Center for Regenerative Medicine (CReM) of Boston University and Boston Medical Center, both US, also used CRISPR technology to create a novel iPSC stem cell line that shone green when differentiated into intestinal cells. This allowed the team to follow the process of intestinal cells differentiation in vitro.
“Generating organoids in our lab allows us to create more accurate disease models, which are used to test treatments and therapies targeted to a specific genetic defect or tissue – and it’s all possible without harming the patient,” said Dr Gustavo Mostoslavsky, co-director of CReM, associate professor of medicine and microbiology at Boston University School of Medicine and faculty in the gastroenterology section at Boston Medical Center. “This approach allows us to determine what treatments could be most effective and which are ineffective, against a disease.”
Using their model, the team generated intestinal organoids from iPSCs containing a mutation that causes cystic fibrosis and corrected the mutation with CRISPR. The intestinal organoids with the mutation did not respond to a drug while the genetically corrected cells did respond, demonstrating their future potential for disease modeling and therapeutic screening applications.
“I hope that this study helps move forward our collective understanding about how diseases impact the gastrointestinal tract at the cellular level. The continual development of novel techniques in creating highly differentiated cells that can be used to develop disease models in a lab setting will pave the way for the development of more targeted approaches to treat many different diseases,” concluded Mostoslavsky.
Related topics
CRISPR, Disease Research, Drug Targets, Organoids, Research & Development, Therapeutics
Related conditions
Colon cancer, Cystic fibrosis, Inflammatory bowel disease (IBD)
Related organisations
Boston Medical Center, Boston University School of Medicine, Center for Regenerative Medicine (CReM) of Boston University and Boston Medical Center
Related people
Dr Gustavo Mostoslavsky