Decoy nanoparticles show success in cell cultures as COVID-19 therapy
Posted: 18 June 2020 | Victoria Rees (Drug Target Review) | No comments yet
Researchers have developed ‘nanosponges’ cloaked in lung cell membranes and macrophage membranes which they found could attract and neutralise COVID-19 in cell cultures.
According to a new study, nanoparticles cloaked in human lung cell membranes and human immune cell membranes can attract and neutralise the SARS-CoV-2 virus in cell culture, causing the virus, which is causing the COVID-19 pandemic, to lose its ability to hijack host cells and reproduce.
The technology was developed by engineers at the University of California (UC) San Diego and tested by researchers at Boston University, both US. Dubbed ‘nanosponges’, the researchers found that the particles can soak up the virus.
In cell culture experiments, the team demonstrated that both types of nanosponges (fragments of the outer membranes of lung epithelial cells and macrophage membrane) caused the SARS-CoV-2 virus to lose nearly 90 percent of its viral infectiousness in a dose-dependent manner.
At a concentration of 5mg per ml, the lung cell membrane-cloaked sponges inhibited 93 percent of the viral infectiousness of SARS-CoV-2. The macrophage-cloaked sponges inhibited 88 percent of the viral infectiousness of SARS-CoV-2.
They also revealed that the nanosponges had angiotensin-converting enzyme 2 (ACE2) and CD147, which are the virus’ natural targets it uses to gain entry into cells, projecting outward from the polymer core.
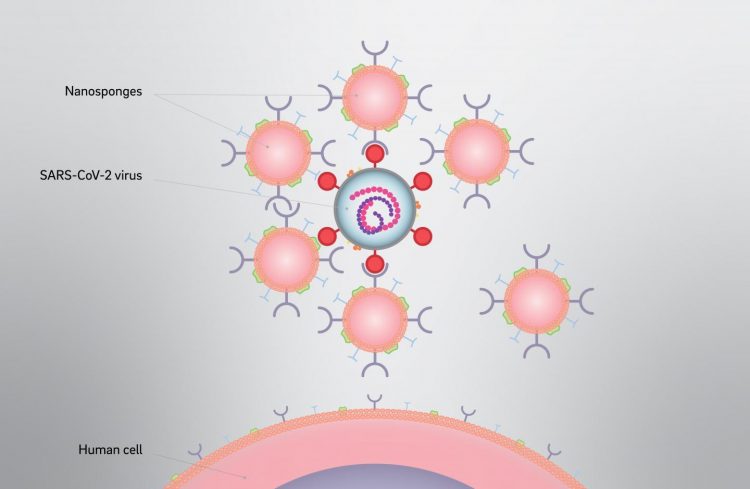
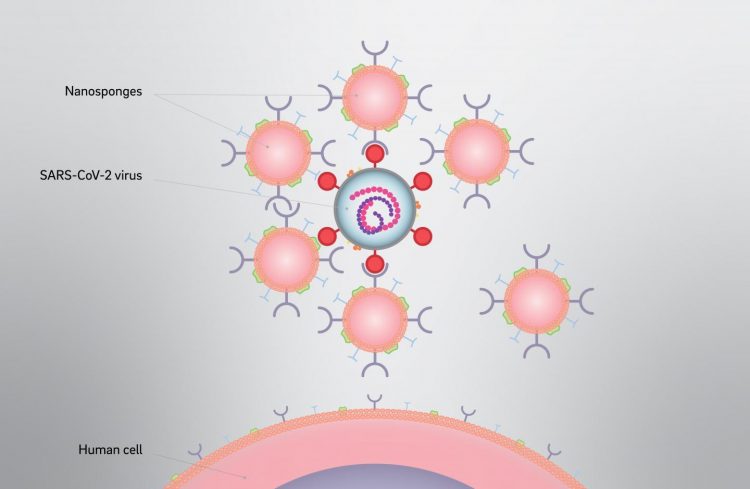
In lab experiments, both the lung cell and immune cell types of nanosponges caused the SARS-CoV-2 virus to lose nearly 90% of its “viral infectivity” in a dose-dependent manner. Viral infectivity is a measure of the ability of the virus to enter the host cell and exploit its resources to replicate and produce additional infectious viral particles [credit: David Baillot/University of California San Diego].
Furthermore, instead of targeting the virus itself, these nanosponges are designed to protect the healthy cells the virus invades. Tested in mice, the team found that their technology did not have any short-term toxicity.
The researchers explain that once the virus binds with a sponge, it loses its viability and is not infectious anymore, so will be taken up by the body’s own immune cells and digested.
“Traditionally, drug developers for infectious diseases dive deep on the details of the pathogen in order to find druggable targets. Our approach is different. We only need to know what the target cells are. And then we aim to protect the targets by creating biomimetic decoys,” said Professor Liangfang Zhang, at the UC San Diego Jacobs School of Engineering.
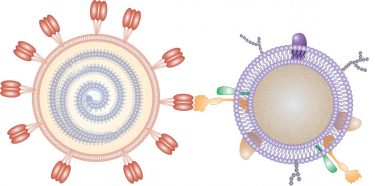
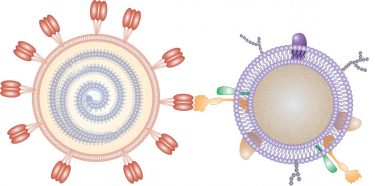
In this illustration, a nanosponge coated with a human cell membrane acts as a decoy to prevent a virus from entering cells [credit: Adapted from Nano Letters 2020, DOI: 10.1021/acs.nanolett.0c02278].
In addition to the encouraging data on neutralising the virus in cell culture, the researchers note that nanosponges cloaked with fragments of the outer membranes of macrophages could have an added benefit: soaking up inflammatory cytokine proteins, which are implicated in some of the most dangerous aspects of COVID-19 and are driven by immune response to the infection.
“From the perspective of an immunologist and virologist, the nanosponge platform was immediately appealing as a potential antiviral because of its ability to work against viruses of any kind. This means that as opposed to a drug or antibody that might very specifically block SARS-CoV-2 infection or replication, these cell membrane nanosponges might function in a more holistic manner in treating a broad spectrum of viral infectious diseases,” said co-first author Associate Professor Anna Honko, at Boston University.
In the next few months, the UC San Diego researchers and collaborators plan to evaluate the nanosponges’ efficacy in animal models. If and when these COVID-19 nanosponges will be tested in humans depends on a variety of factors, but the researchers say they are moving as fast as possible.
“Another interesting aspect of our approach is that even as SARS-CoV-2 mutates, as long as the virus can still invade the cells we are mimicking, our nanosponge approach should still work. I’m not sure this can be said for some of the vaccines and therapeutics that are currently being developed,” said Zhang.
The study was published in Nano Letters.
Related topics
Cell Cultures, Drug Targets, Nanomedicine, Nanoparticles, Nanotechnology, Research & Development, Therapeutics, Toxicology
Related conditions
Coronavirus, Covid-19
Related organisations
Boston University, University of California San Diego
Related people
Associate Professor Anna Honko, Professor Liangfang Zhang