Rare autoantibody diseases: an innovative targeted pathway
Posted: 7 July 2023 | Dr Katie Abouzahr | No comments yet
Dr Katie Abouzahr outlines how precision targeting utilising the neonatal fragment crystallisable receptor pathway may provide accessible new treatments for autoantibody diseases.
Dr Katie Abouzahr, Vice President, Autoantibody Portfolio Development Leader at the Janssen Pharmaceutical Companies of Johnson & Johnson, outlines how precision targeting in drug development utilising the neonatal fragment crystallisable (Fc) receptor (FcRn) pathway may provide accessible new treatments for rare autoantibody diseases and beyond.
Approximately three percent of the global population — 240 million people — experience autoantibody diseases, which occur when one’s own body attacks critical organs and tissues. In pregnant individuals, maternal autoantibodies can even attack the organs and tissues of the foetus, 1-9 Many of these diseases are rare, with no safe, targeted, advanced and effective treatment options approved for patients in need.
Antibodies are proteins that guard against foreign substances that enter our bodies,such as bacteria, fungi, viruses and toxins. Antibodies protect us by attaching to molecules on those invaders (known as antigens) and triggering our body’s natural immune response to destroy them.
We can think of autoantibodies as misguided, or pathogenic, antibodies: instead of reacting to foreign antigens, they respond to our body’s own proteins. This can create an abnormal immune response that attacks the cells of our bodies and contributes to the development of autoantibody diseases. This can occur during pregnancy, when a pregnant person forms certain antibodies — termed alloantibodies — that attack the foetus’ blood cells and/or organs.
Autoantibody diseases comprise a large and varied group of more than 80 chronic conditions. Janssen Immunology considers these diseases within three pillars:10-13
- Maternal-foetal diseases such as haemolytic disease of the foetus and newborn (HDFN), in which a pregnant person forms alloantibodies to the foetus’ red blood cells, causing their destruction, which can result in haemolysis, anaemia, and in about one-quarter of cases, foetal death
- Rare autoantibody diseases directly mediated by autoantibodies. These include warm autoimmune haemolytic anaemia (wAIHA), which involves the premature destruction of healthy red blood cells; myasthenia gravis (MG), a disorder characterised by fluctuating weakness in the skeletal muscles; chronic inflammatory demyelinating polyneuropathy (CIDP), a neurological disorder characterised by progressive weakness and impaired sensory function in the limbs; idiopathic inflammatory myopathies (IIM), a group of disorders characterised by inflammation of skeletal muscles; and bullous pemphigoid (BP), a rare condition that causes large, fluid-filled blisters on the skin
- Prevalent rheumatologic diseases mediated by autoantibody complexes, such as rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), and Sjögren’s disease (SjD).
Autoantibody diseases represent a significant area of unmet patient need wherein the limited number of available interventions for most autoantibody diseases can be suboptimal. This means that physicians and patients are sometimes required to utilise approaches that are often not approved for these diseases, are non-specific, lack adequate efficacy for the specific disease state, may require invasive procedures, are often associated with safety and tolerability issues, and may have detrimental long-term effects.
There is a clear need for new and approved, safe, effective and innovative targeted therapies to address the underlying causes of autoantibody diseases.
The power of precision therapy
Targeted — or precision — therapy, a technique that has been honed for many years in cancer treatment, is now being applied in a wider context. Precision medicine is a healthcare approach that uses diagnostic tests, imaging and health information from patients to prevent or treat disease. With in-depth information at the cellular level, relevant to a patient’s disease or condition, we can identify the distinct patient populations most likely to benefit from a specific treatment, in contrast to the traditional ‘one size fits all’ approach.14 This precision methodology has been facilitated by our increased understanding of the immune system and molecular mechanisms of disease.
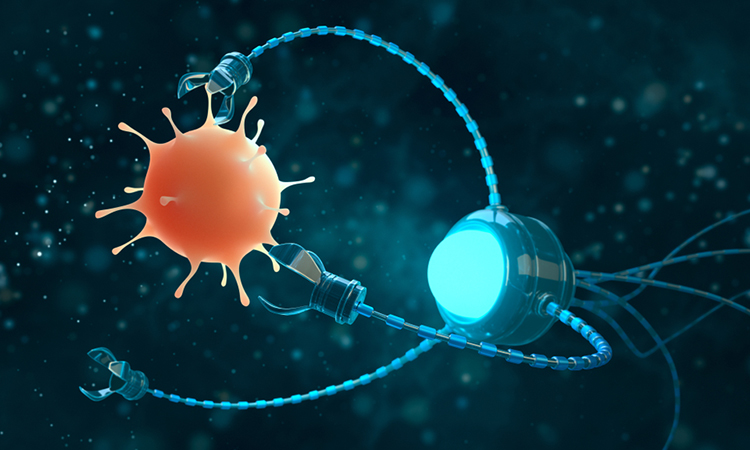
Targeted therapies are designed to interfere with, or target, molecules such as proteins within the body. In some cases, the drug will attach to the molecule it targets, preventing it from doing its job. Other times, the drug will physically block the molecule from the place it normally goes. By stopping or blocking the normal work of these molecules, diseases can often be slowed or even stopped.
A critical benefit of targeted therapy is that it can deliver safe and effective treatment, while maintaining the health and efficacy of the rest of the immune function. Simply put, it achieves the goal of providing the right treatment for the right patient at the right time with the right dose.
The FcRn pathway
An innovative approach to achieving the benefits of targeted therapy across many diseases is a targeted pathway approach, which we are employing at Janssen. While traditional drug discovery utilised a one-drug, one-disease approach, a pathway approach assumes that targeting a particular mechanism — ie, a gene or protein within the immune system function — can potentially treat multiple diseases impacted by that mechanism with a single therapy.
A promising new target in autoantibody disease research is a protein called the neonatal fragment crystallisable (Fc) receptor (FcRn), a transmembrane protein that is present throughout life, located mostly inside vesicles within endothelial and immune cells. It normally binds to and recycles internalised immunoglobin G (IgG) antibodies, which are important for fighting infections, as well as albumin, which helps move many small molecules through the blood. The result of this ‘recycling’ is that FcRn increases levels of IgG by preventing the body from breaking it down. New research has suggested that blocking FcRn may disrupt the progression of various diseases that are driven by IgG autoantibodies.15
Promising possibilities in maternal-foetal health
New insights into the FcRn pathway are unlocking opportunities to revolutionise maternal-foetal immunology, including how the rare and potentially devastating antibody-mediated illness HDFN is addressed.16 Although diagnostic tests and preventative medical advances have reduced HDFN incidence and severity in recent decades, HDFN still occurs in up to 80 in every 100,000 pregnancies in the US.17
HDFN occurs when there is a mismatch between red blood cell antigens of the pregnant person and foetus. However, not all mismatches lead to severe HDFN; for HDFN to occur, the foetus must be antigen positive (inherited from the paternal side) and the pregnant person must be antigen negative.18 There are numerous different antigens on red blood cells that may lead to HDFN in the event there is a mismatch, such as blood type (ABO), Rhesus (Rh) factor (D, c, C, E, e), Kell, Kidd, Duffy, MNS and s.
In HDFN, the pregnant person’s immune system mounts an immune response against the foetus’ red blood cells by creating maternal IgG alloantibodies which enter the foetal circulation through the placenta and destroy the red blood cells of the foetus. These alloantibodies are transported along with general maternal IgG across the placenta via the neonatal FcRn pathway – an FcRn function specific to pregnancy that is distinct from the recycling activity it conducts throughout life as described above.16,17
There are currently no approved therapeutics for the treatment of HDFN. Pregnancies at risk of severe HDFN may develop life-threatening foetal anaemia, which requires highly invasive procedures — intrauterine blood transfusions (IUTs) — to the foetus. If not managed in a timely manner by a knowledgeable and skilled expert, the anaemic foetus may develop severe foetal hydrops, a condition in which large amounts of fluid build up in the foetus’ tissues and organs, causing extensive swelling (edema) with life-threatening consequences. IUTs are technically complex, requiring access to specialists with significant skill and expertise, and even then, severe procedure-related complications can still occur.
After delivery, newborns retain maternal alloantibodies for several weeks and are at risk of severe jaundice, anaemia and other related complications which can also be life-threatening. As a result, severe HDFN causes significant maternal-foetal and neonatal morbidity, mortality, and in rare cases, irreversible neurodevelopmental deficits in the neonate and infant.
Thus, the need for safer, effective and non-invasive treatment options for HDFN are critical. Fortunately, research advancements are allowing us to gain better understanding of the disease and ways we can help to address it. Early research in pregnant women at risk of HDFN shows that an FcRn-blocking therapy may remove antibodies from circulation and, in pregnancy, prevent them from reaching the foetus and causing this condition.18 This type of success in treatment could be life-changing for the families who have been and could be impacted by HDFN.
Developing solutions
A significant barrier to the development of novel therapies and treatment paradigms for immune-mediated diseases has been the complexity and heterogeneity of these diseases, which consist of different disease states with distinct unmet medical needs and biology.19 Yet through scientific advances in the understanding of disease pathophysiology in different tissues and organs, and the identification of biomarkers for informed stratification of diseases, we can now work towards developing new medicines with targeted mechanisms of action tailored to differentiated patient populations.
For autoantibody diseases, new discoveries in immunology are leading to profound learnings about drivers of disease, helping us to expand the development of medicines more rapidly and effectively. A critical part of being able to expand development is through our pathway approach to drug development: developing targeted therapies that can treat multiple diseases affected by one mechanism.
The opportunities for targeted therapy are many and the research is incredibly exciting. We continue to support the growing body of research being developed to meet the needs of the millions of patients awaiting solutions.
Author Bio:
 Dr Katie Abouzahr
Dr Katie Abouzahr
Katie Abouzahr, M.D., Vice President, Autoantibody Portfolio and Maternal Fetal Disease Area Leader. She is passionate about transforming healthcare for women and addressing unmet needs in the maternal-fetal immunology space.
References
- Prevalence of rare diseases by alphabetical list [Internet]. orphanet. 2021 [cited 2023Feb28]. Available from: https://www.orpha.net/orphacom/cahiers/docs/GB/Prevalence_of_rare_diseases_by_alphabetical_list.pdf
- Osanan GC, Silveira Reis ZN et al. Predictive factors of perinatal mortality in transfused fetuses due to maternal alloimmunization: What really matters? The Journal of Maternal-Fetal & Neonatal Medicine. 2011;25(8):1333–7.
- Gilhus NE, Tzartos S, Evoli A, et al. Nature Reviews Disease Primers. 2019;5(1).
- Bacci ED, Coyne KS, et al. Understanding side effects of therapy for myasthenia gravis and their impact on daily life. BMC Neurology. 2019;19(1).
- Menon D, Barnett C, Bril V. Novel treatments in Myasthenia Gravis. Frontiers in Neurology. 2020;11.
- Schett G, Teitelbaum SL. Osteoclasts and arthritis. Journal of Bone and Mineral Research. 2009;24(7):1142–6.
- Kocijan R, Harre U, Schett G. ACPA and bone loss in rheumatoid arthritis. Current Rheumatology Reports. 2013;15(10).
- Sieghart D, Platzer A et al. Determination of autoantibody isotypes increases the sensitivity of serodiagnostics in rheumatoid arthritis. Frontiers in Immunology. 2018;9.
- Deane KD, Holers VM. The natural history of rheumatoid arthritis. Clinical Therapeutics. 2019;41(7):1256–69.
- Eggert M, Zettl UK, Neeck G. Autoantibodies in autoimmune diseases. Current Pharmaceutical Design. 2010;16(14):1634–43.
- Ludwig RJ, Vanhoorelbeke K, Leypoldt F, Kaya Z, Bieber K, McLachlan SM, et al. Mechanisms of autoantibody-induced pathology. Frontiers in Immunology. 2017;8.
- Bender M, Christiansen J, Quick M. The terrible toll of 76 autoimmune diseases [Internet]. Scientific American. Scientific American; 2021 [cited 2023Feb28]. Available from: https://www.scientificamerican.com/article/the-terrible-toll-of-76-autoimmune-diseases/
- Hayter SM, Cook MC. Updated assessment of the prevalence, spectrum and case definition of autoimmune disease. Autoimmunity Reviews. 2012;11(10):754–65.
- Precision medicine [Internet]. EFPIA Homepage. [cited 2022Dec]. Available from: https://www.efpia.eu/about-medicines/development-of-medicines/precision-medicine/#/
- Neely Mozaffarian. Advancing maternal-fetal immunology by unlocking new insights into immune pathways [Internet]. MDedge ObGyn. 2022. Available from: https://www.mdedge.com/obgyn/article/248841/advancing-maternal-fetal-immunology-unlocking-new-insights-immune-pathways
- Romanowska-Próchnicka K, Felis-Giemza A, et al. The role of TNF-α and anti-TNF-α agents during preconception, pregnancy, and breastfeeding. International Journal of Molecular Sciences. 2021;22(6):2922.
- Delaney M, Matthews DC. Hemolytic disease of the fetus and newborn: Managing the mother, fetus, and newborn. Hematology. 2015;2015(1):146–51.
- Mari G, Norton ME, Stone J, Berghella V, Sciscione AC, Tate D, et al. Society for Maternal-Fetal Medicine (SMFM) clinical guideline #8: The fetus at risk for anemia–diagnosis and management. American Journal of Obstetrics and Gynecology. 2015;212(6):697–710.
- Varadé J, Magadán S, González-Fernández Á. Human immunology and immunotherapy: Main achievements and challenges. Cellular and Molecular Immunology. 2020;18(4):805–28.
Related topics
Antibody Discovery, Drug Delivery, Drug Development, Precision Medicine, RNAs, Targets, Therapeutics
Related organisations
Janssen
Related people
Dr Katie Abouzahr