Engineered airway lining created to study how COVID-19 affects respiratory tracts
Posted: 11 February 2022 | Ria Kakkad (Drug Target Review) | No comments yet
Researchers have made a respiratory model of COVID-19, made from patient-derived stem cells, to understand how the virus affects respiration and which could be used to test possible drugs.
A three-dimensional (3D) airway model, made from patient-derived stem cells, has been developed by a team at Boston Children’s Hospital, US to potentially provide answers about the preliminary stages of COVID-19 infection. The model not only replicates the infection process but can be used to assess possible antiviral drugs.
“Human primary bronchial cells are the gold standard for studying lower respiratory infections, but the value of our model is that it does not require getting tissue from patients’ airways, an invasive procedure,” said Dr Ruby Wang, attending physician in Boston Children’s Division of Pulmonary Medicine. “Our platform provides an inexhaustible supply of cells for modelling purposes and produces the relevant airway cell types.”
To build the model, the team obtained blood cells from two individuals and genetically “reprogrammed” them back to a stem cell state. They then added factors to get the stem cells to form all the major types of epithelial cells that line the trachea and bronchi, including multi-ciliated, secretory and basal cells. The hallmark cell receptor ACE2 was present in the stem-cell-derived airways, as was TMPRSS2, a key enzyme that aids in viral entry.
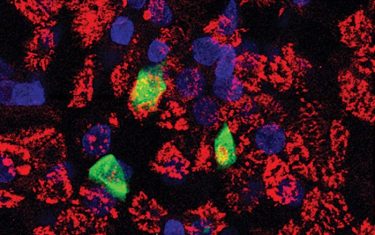
Derived from patients’ cells, a new airway model containing ciliated respiratory endothelial cells recapitulates sars-cov-2 infection and can be used to test drugs. Three ciliated cells in this model are infected with the virus.
[Credit: Chantelle Simone Roach, Boston Children’s, and Jake La Suer, Boston University.]
Using live SARS-CoV-2, the team successfully infected the model airway and showed that multi-ciliated airway cells are the initial point of viral entry.
“That is important, because ciliated cells have an important function in propelling airway mucus and entrapped pathogens up away from the lungs,” said Wang. “If the ciliated cells are injured, the virus can be more easily propelled down to the lower lung.”
Once infected, the model airway mounted a robust antiviral response, producing type 1 and type 3 interferons. The team also observed a marked inflammatory response, with increased production of inflammatory signalling molecules and increased expression of interferon-stimulated genes and genes involved in activating immune cells.
As the model airway genetically matches the patient from whom it is derived, it lends itself to testing how COVID-19 affects patients with specific underlying conditions that may affect their susceptibility. The team are also currently using stem cells from cystic fibrosis (CF) patients to study how a CF airway responds to SARS-CoV-2 and other pathogens.
Most importantly, the model can also be used to test possible treatments for COVID-19. The researchers assessed the antiviral remdesivir and found a decrease in viral replication. They found the same when they evaluated camostat mesylate, which inhibits TMPRSS2, confirming that the virus requires TMPRSS2 to infect airway cells.
The team’s findings are described in the journal American Journal of Physiology – Lung Cellular and Molecular Physiology. In the future, Wang plans to use the airway model to study Omicron, Delta and other new variants and their response to treatments in both healthy patients and those with airway diseases such as CF.
Related topics
Disease Research, Drug Discovery Processes, Organoids, Stem Cells, Targets, Therapeutics
Related conditions
Coronavirus, Covid-19
Related organisations
Boston Children's Hospital
Related people
Dr Ruby Wang