Possible connection between HIV and tuberculosis revealed
Posted: 17 February 2022 | Ria Kakkad (Drug Target Review) | No comments yet
A recent study has shown that antiretroviral therapy timing impacts the animal version of HIV and latent tuberculosis.


Researchers from the Texas Biomedical Research Institute and National Primate Research Center, both US, found that two weeks can make a significant difference in treating the animal version of HIV and latent tuberculosis (TB). The breakthrough, published in the Journal of Clinical Investigation, could help in the development of therapies and a combined vaccine for the two diseases in humans.
“Most humans are able to control a low dose of TB infection by maintaining it in a dormant form called latent TB infection,” said Dr Riti Sharan, a staff scientist at Texas Biomedical Research Institute. “But if they get co-infected with HIV, then there is a high possibility that TB is reactivated and the patient ultimately dies of TB. Our objective is to improve existing interventions or identify new ones to prevent latent TB from being reactivated.”
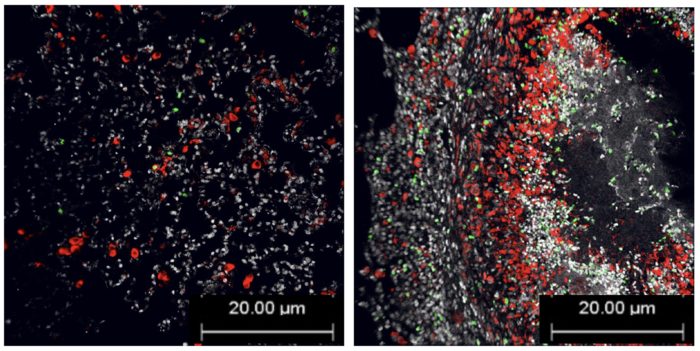
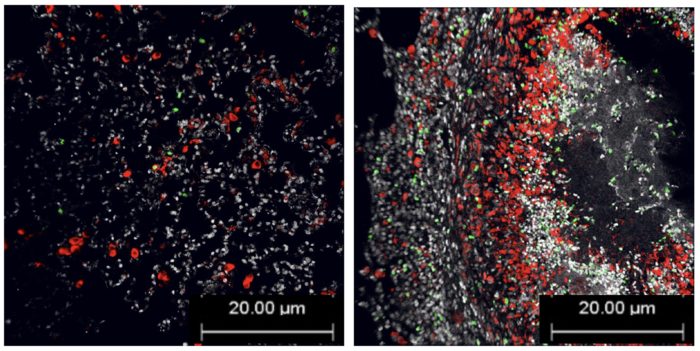
Lung tissue of animals with TB that started cART two weeks post SIV infection (left) versus at four weeks post SIV infection (right). There are far fewer green spots on the left, which indicate fewer macrophages are dying and latent TB is kept more under control, thanks to starting cART earlier. Red spots are also macrophages.
[Credit: Texas Biomed.]
The research team studied what happened in humans using non-human primates, which contract simian immunodeficiency virus (SIV), the monkey version of HIV, as well as TB. The researchers found that when animals with a latent TB infection start combined antiretroviral therapy (cART) against SIV two weeks after infection, the animals fare much better than if cART is started at four weeks post SIV infection. In the group that started cART at two weeks post infection, chronic immune activation was significantly reduced, as was SIV replication and latent TB was not reactivated as much as in the group that started cART four weeks post infection. In fact, the lungs in the group that started treatment at four weeks looked more like they were not receiving any treatment at all.
The researchers highlight that the difference of two weeks may not directly apply to humans – in part because most people are unlikely to be diagnosed and begin treatment for HIV within two weeks of infection. However, the real value of the finding is identifying chronic immune activation as the main driver of latent TB reactivation following HIV infection. The researchers are now able to study possible mechanisms for protection.
“Ultimately, we aim to use this information to design a therapy that would enable patients to prevent latent TB reactivation by limiting the HIV-driven chronic immune activation,” Sharan said.
Related topics
Antiretroviral Therapies, Disease Research, Drug Repurposing, Therapeutics, Vaccine
Related conditions
HIV, Tuberculosis, Tuberculosis (TB)
Related organisations
National Primate Research Center, Texas Biomedical Research Institute
Related people
Dr Riti Sharan







