Novel CAR T-cell therapy could help cure HIV
Posted: 1 September 2020 | Hannah Balfour (Drug Target Review) | No comments yet
The designers of the Dual Chimeric Antigen Receptor (CAR) T cell therapy report it slows HIV replication and leads to a smaller viral reservoir in HIV-infected mice.
Researchers have designed a novel Dual Chimeric Antigen Receptor (CAR) T-cell therapy that could be used to cure Human Immunodeficiency Virus (HIV).
The global HIV epidemic is thought to impact more than 35 million people. The currently available treatment, antiretroviral therapy (ART), is a daily medication regimen that can only control, not cure, the disease. As a result, access and lifelong adherence to the treatment is a significant barrier for many living with HIV.
Holding back the development of a cure for HIV is the viral reservoir; copies of the HIV genome inserted into the host genome in infected cells, which – if ART is stopped – can rapidly be copied to create new viral particles and ultimately lead to the development of acquired immunodeficiency syndrome (AIDS).
In order to overcome this barrier, US researchers led by Dr Todd Allen, a professor of Medicine at Harvard Medical School (HMS) and group leader at the Ragon Institute of Massachusetts General Hospital (MGH), MIT and Harvard; and Dr Jim Riley, a professor of Microbiology in the Perelman School of Medicine at the University of Pennsylvania, developed a Dual CAR T-cell immunotherapy that can help fight HIV infection.
Riley commented that the study published in Nature Medicine: “highlights how relatively straightforward alterations to the way T cells are engineered can lead to dramatic changes in their potency and durability.” He added that the findings have “significant implications for using engineered T cells to fight both HIV and cancer.”
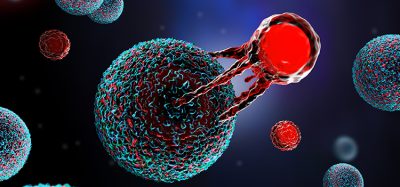
CAR T cells are a type of immunotherapy, currently used in cancer treatments, in which a patient’s own immune T cells are engineered to express CARs. These CARs re-programme the T cells to recognise and eliminate specific diseased or infected cells, such as cancer cells or, in this instance, HIV-infected cells.
The research groups collaborated on the design of a new HIV-specific CAR T cell. They needed to create a CAR T cell able to target and quickly eliminate HIV-infected cells, survive and reproduce in vivo and resist infection by HIV, since HIV’s primary target is T cells.
“By using a stepwise approach to solve each issue as it arose, we developed protected Dual CAR T cells, which provided a strong, long-lasting response against HIV-infection while being resistant to the virus itself,” Allen said.
The Dual CAR T cell was made by engineering two CARs into a single T cell. Each CAR had a CD4 protein that allowed it to target HIV-infected cells and a costimulatory domain, which signalled the CAR T cell to increase its immune functions. The first CAR contained the 4-1BB co-stimulatory domain, which stimulates cell proliferation and persistence, while the second has the CD28 co-stimulatory domain, which increases its ability to kill infected cells.
To protect their CAR T cells from HIV infection, they also added in a protein called C34-CXCR4, developed in the lab of Dr James Hoxie, a professor of Hematology-Oncology at Penn Medicine. C34-CXCR4 prevents HIV from attaching to and infecting cells. With this attachment, the final CAR T cell was long-lived, replicated in response to HIV infection, killed infected cells effectively and was partially resistant to HIV infection.
When the Dual CAR T cells were given to HIV-infected mice, the team observed that HIV replication was slower and the animals had fewer HIV infected cells than their untreated counterparts. They also reported reduced amounts of virus and preservation of CD4+ T cells, HIV’s preferred target, in the blood of these animals. In addition, when they combined Dual CAR T cells with ART in HIV-infected mice, the virus was suppressed faster, leading to a smaller viral reservoir than in mice treated with ART alone.
“The ability of these protected Dual CAR T cells to reduce the HIV burden in a variety of tissues and cell types, including long-lived memory CD4+ T cells, we believe supports the approach of using CAR T cell therapy as a new tool to target the HIV reservoir towards a functional cure for HIV,” concluded Allen.
Related topics
Antiretroviral Therapies, Chimeric Antigen Receptors (CARs), Drug Development, Drug Targets, Immunotherapy, In Vivo, Research & Development, T cells, Therapeutics
Related organisations
Harvard Medical School (HMS), Penn Medicine, Perelman School of Medicine at the University of Pennsylvania, Ragon Institute of Massachusetts General Hospital (MGH) MIT and Harvard
Related people
Dr James Hoxie, Dr Jim Riley, Dr Todd Allen