New drug target identified for myelodysplastic syndrome
Posted: 8 October 2021 | Anna Begley (Drug Target Review) | No comments yet
Researchers have uncovered how mutations affecting RNA splicing alter cells to develop myelodysplastic syndrome (MDS).
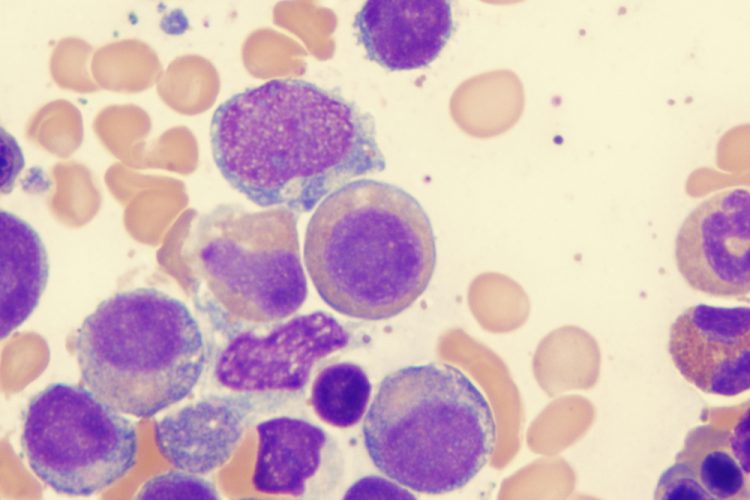
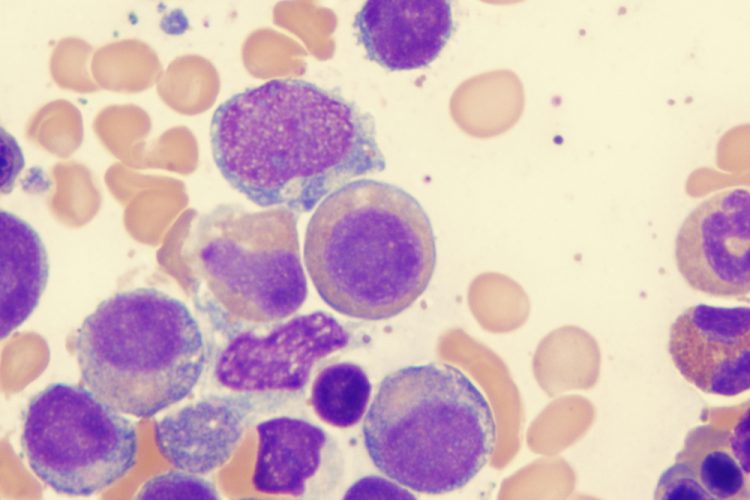
A team at Mount Sinai Hospital and the University of California (UC) San Diego, both US, have shown for the first time how mutations affecting a cellular process called RNA splicing alter cells to develop myelodysplastic syndrome (MDS) and other haematological malignancies and solid tumours.
Their research, published in Cancer Discovery, found that these mutations produce an alternative version of the protein created by the gene known as GNAS. This protein can be targeted by drugs already approved by the US Food and Drug Administration (FDA) for treating other cancers and therefore could be a suitable target in MDS. The researchers are creating a clinical trial to test these drugs, known as MEK inhibitors and named for the proteins they inhibit to stop cancer.
“This is the first study to discover that the altered protein created by GNAS is increased in cells with these mutations in MDS and this results in the activation of processes that would render the cancer cells vulnerable to the MEK inhibitors,” stated co-senior author and associate professor Eirini Papapetrou. “The discovery that we can try to use MEK inhibitors in this cancer is also a first and our findings also support future drug development to target GNAS, identified in this study.”
The researchers then generated models of the mutations using stem cells in order to study them in a physiological genetic context. They subsequently turned the engineered cells into haematopoietic progenitor cells which are the relevant cell type in blood cancers and performed splicing and RNA binding analyses. “This work integrates isogenic models of disease with cutting-edge RNA-omics to converge onto a new target for MDS,” explained Professor Gene Yeo.
ARTICLE: Telomerase – a universal cancer target for immunotherapeutic vaccines
These analyses allowed the team to identify high-confidence targets and to identify the driver of the disease. They showed that MDS cells from the model as well as cells from MDS patients with these mutations were sensitive to treatment with MEK inhibitors, suggesting an exciting new avenue for future treatments.
Related topics
Drug Targets, Genomics, Molecular Biology, Molecular Targets, Oncology, Protein, Stem Cells, Target Molecule, Therapeutics
Related conditions
Myelodysplastic syndromes (MDS)
Related organisations
Mount Sinai Hospital, UC San Diego
Related people
Associate Professor Eirini Papapetrou, Professor Gene Yeo








