Fighting HIV: could antibodies be the answer?
Posted: 1 April 2021 | Victoria Rees (Drug Target Review) | No comments yet
Although a cure for HIV continues to elude scientists, strategies to control the virus and immunise people are developing at rapid pace. Here, Drug Target Review’s Victoria Rees discusses why researchers are focusing on antibodies as approaches to combat HIV and highlights recent findings from two pre-clinical studies into how antibodies can be used as treatments and prophylactics for the virus.
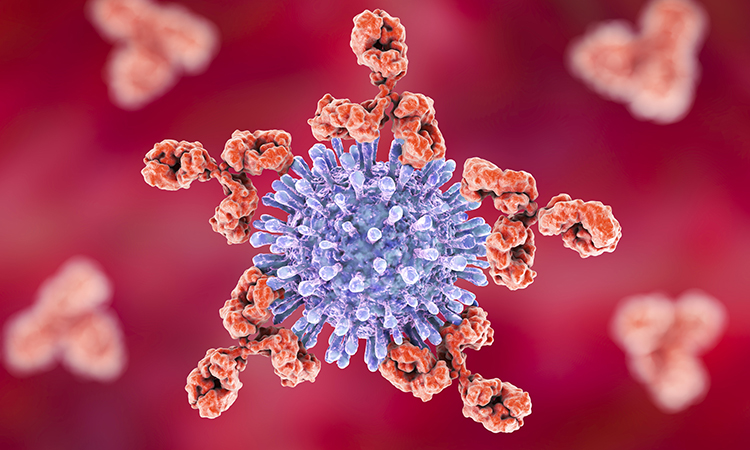
IN 2019, THERE WERE approximately 38 million people across the globe living with HIV/AIDS, according to the World Health Organization (WHO). Having claimed the lives of 33 million people so far,1 there is currently no cure or vaccine available to treat or prevent the disease.
During the lifecycle of HIV, the virus incorporates itself into its host cell’s DNA. While antiretroviral therapies such as post-exposure prophylaxis (PEP) can prevent the spread of the virus that might be produced from infecting new cells, it cannot eliminate viral DNA from the host cell’s genome. HIV’s ability to hide its instructions inside cells means that drugs cannot reach it, allowing it to escape cure.2
Due to HIV’s highly-variable nature, it is also easy for the virus to target and impair immune cells, integrating into the host genome early in infection and establishing latent infection. No infected individuals have ever developed an immune response that completely cleared their infection, making it difficult for scientists to determine what constitutes an appropriate immune response to HIV,3 thus hindering the development of a vaccine.
The potential of antibodies
To address these challenges, researchers have turned to antibodies as a possible solution. One antibody strategy being explored for HIV treatment is broadly neutralising antibodies (bNAbs). These are thought to be robust candidates for treatment and vaccines because they trigger few side effects and can be modified to ensure they remain in the body for a long time. bNAbs that target HIV can bind the virus and prevent it from entering the cell, speeding up its elimination. They can also bind an HIV-infected cell and stimulate immune system components that enable the destruction of the cell.3


Nineteen novel bNAbs, which are being tested and optimised in pre-clinical trials at present, have already proven to be more potent and broad-acting than pre-exposure prophylaxis (PrEP) – the pre‑emptive use of antiretroviral therapy by individuals at risk of contracting the virus.4
Currently, a bNAb called VRC01 is being studied in a clinical trial,4 having been discovered by researchers at the US National Institute of Allergy and Infectious Disease (NIAID), part of the National Institutes of Health (NIH). This bNAb is being delivered as an intravenous infusion to prevent HIV in individuals. Another significant development from scientists at the NIAID Vaccine Research Center was the discovery of a promising antibody called vFP16.02, which stimulated an immune response and has the potential to effectively fight HIV.5
Therefore, an increasing number of studies are turning to bNAbs as a potential source of HIV treatment or vaccines, due to their apparent benefits over conventional antiretroviral therapies or even prophylactics.
Antibodies for HIV treatment
According to the researchers from the US Military HIV Research Program (MHRP), a critical barrier to curing HIV is the reservoir of latent virus that remains hidden and infects cells throughout the body, leading to viral rebound in the vast majority of HIV-infected individuals after they discontinue antiretroviral therapy.
An increasing number of studies are turning to bNAbs as a potential source of HIV treatment”
“It has become clear that we need a combination intervention strategy to generate longer lasting viral suppression,” said Dr Sandhya Vasan, a Director for the MHRP.
To address these issues, a study led by MHRP researchers tested an experimental therapy combining a TLR7 agonist, GS-986, and two bNAbs, N6-LS and PGT121. The team hypothesised that the TLR7 agonist, supported by therapeutic bnAbs, would stimulate the immune system to clear latent HIV.
They found the combination therapy was able to delay viral rebound in SHIV-infected macaques after antiretroviral therapy interruption. Their findings were published in PLOS Pathogens.6
In the study, the rhesus macaques were initiated on viral suppressive antiretroviral therapy 14 days post-infection, a timespan from infection to treatment that the researchers say mirrors what is feasible in acute HIV infection. The team then administered the combination therapy, which targeted different regions of the HIV envelope. This was followed by a pause in antiretroviral therapy, allowing the researchers to measure how long it took for the SHIV viral load to rebound.
“This study demonstrated that the combination of TLR7 agonist and dual bnAbs delayed viral rebound after antiretroviral therapy interruption by two-fold,” said Dr Denise Hsu, MHRP Associate Director of Therapeutics. “This approach may represent a potential strategy to target the HIV reservoir in HIV-infected individuals.”
Based on these new pre-clinical data, the MHRP hopes to evaluate the combination of innate immune stimulation, active and passive immunisation for the induction of HIV remission in early treated people living with HIV.
Antibodies in HIV vaccines
Findings published in Proceedings of the National Academy of Sciences (PNAS)7 demonstrated that the previously mentioned vFP16.02-like immune response could be used as the basis for an eventual vaccine against HIV. A team at the NIAID Vaccine Research Center partnered with the Immune Engineering Laboratory at the University of Kansas, US, to understand how antibody-based approaches could be developed in the fight against diverse HIV antigens.


The scientists identified several important mechanistic features about immune protection, including the binding strength of the antibody directly correlated to its ability to neutralise HIV.
“We wanted to see whether we could further increase the potency and neutralisation breadth of this antibody,” said co-lead author Bharat Madan, a postdoctoral who also led the work. “That means you could give a lower amount of antibody to someone as a prophylaxis and it would produce a much better and broader immune response.”
Madan and colleagues used high-throughput screening platforms based on modified yeast cells to display antibody variant proteins and advanced cell sorting. They also used next-generation DNA sequencing to explore a vast library of possible alterations, or mutations, to the vFP16.02 antibody. They then analysed the antibodies’ response against 208 different HIV strains.
The research focused on improving structural and biophysical features in the antibodies that bind to the HIV fusion peptide, a vulnerable site on HIV-1.
“There are certain regions on this antibody which are more prone to accept the mutation that can enhance the binding affinity towards the fusion peptide,” Madan said. “We found a variant or a mutation – a cluster towards the bottom portion of the antibody we call the framework region – that can enhance binding strength and that correlates not towards a particular variant, but to more diverse HIV strains as well.”
Although there are no approved cures or vaccines for HIV, new treatments and prophylactics are on the horizon”
The most effective variants in the library of mutants boosted the ability of vFP16.02 to recognise and bind to both soluble fusion peptides and the full HIV-1 envelope protein. These antibody variants, which had mutations concentrated in antibody framework regions, achieved up to 37 percent neutralisation breadth compared to 28 percent neutralisation of the unmodified vFP16.02 antibody.
“[This study] reveals some of the key insights in how to best target HIV-1 proteins in the next generation of vaccine designs,” said Assistant Professor Brandon DeKosky, whose lab conducted the research.
Although there are no approved cures or vaccines for HIV, new treatments and prophylactics are on the horizon. Whether focusing on bNAb technologies or building upon previous research, researchers are making progress in the fight against HIV. Their next steps will be to continue the development of antibody-based therapies that will hopefully one day reach the clinic.
About the author
Victoria Rees is the Deputy Editor of Drug Target Review.
References
- HIV/AIDS [Internet]. Who.int. 2021 [cited 12 March 2021]. Available from: https://www.who.int/news-room/fact-sheets/detail/hiv-aids
- HIV 101 [Internet]. Science of HIV. 2021 [cited 12 March 2021]. Available from: http://scienceofhiv.org/wp/?page_id=18
- The current and future landscape of HIV treatments and vaccines [Internet]. European Pharmaceutical Review. 2021 [cited 12 March 2021]. Available from: https://www.europeanpharmaceuticalreview.com/article/143332/the-current-and-future-landscape-of-hiv-treatments-and-vaccines/
- HIV [Internet]. ICON plc. 2021 [cited 12 March 2021]. Available from: https://www.iconplc.com/insights/therapeutics/hiv/
- Researchers boost the potency of an HIV-1 antibody, tracing new potential pathways for vaccine development [Internet]. 2021 [cited 12 March 2021]. Available from: https://news.ku.edu/2021/03/08/researchers-boost-potency-hiv-1-antibody-tracing-new-potential-pathways-vaccine
- Hsu D, Schuetz A, Imerbsin R, Silsorn D, Pegu A, Inthawong D et al. TLR7 agonist, N6-LS and PGT121 delayed viral rebound in SHIV-infected macaques after antiretroviral therapy interruption. PLOS Pathogens. 2021;17(2):e1009339.
- Madan B, Zhang B, Xu K, Chao C, O’Dell S, Wolfe J et al. Mutational fitness landscapes reveal genetic and structural improvement pathways for a vaccine-elicited HIV-1 broadly neutralizing antibody. Proceedings of the National Academy of Sciences. 2021;118(10):e2011653118.
Related topics
Antibodies, Biopharmaceuticals, Disease Research, Protein, Proteomics
Related conditions
HIV
Related organisations
University of Kansas, US Military HIV Research Program (MHRP), US National Institute of Allergy and Infectious Diseases (NIAID), US National Institutes of Health (NIH), World Health Organization (WHO)
Related people
Assistant Professor Brandon DeKosky, Bharat Madan, Dr Denise Hsu, Dr Sandhya Vasan