N439K variant of SARS-CoV-2 is resistant to some neutralising antibodies, shows study
Posted: 1 February 2021 | Hannah Balfour (Drug Target Review) | No comments yet
The N439K mutation improves the interaction between SARS-CoV-2 Spike protein and the viral receptor ACE2 and eludes antibody-mediated immunity, say investigators.
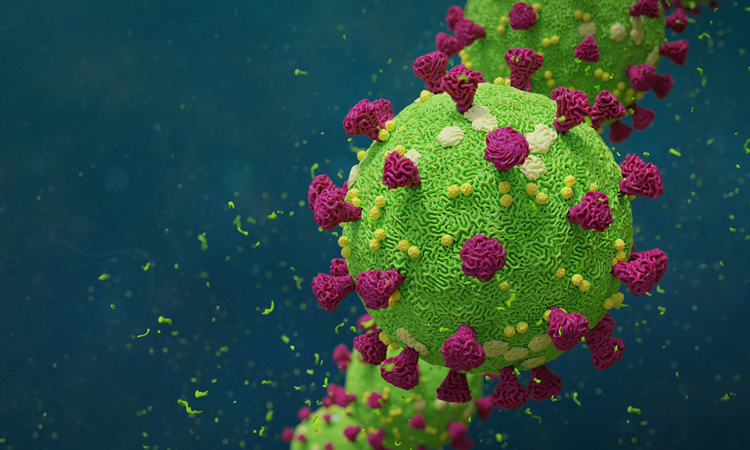
According to researchers, a single change to the amino acid structure of the SARS-CoV-2 Spike (S) protein increases its affinity for the angiotensin-converting enzyme 2 (ACE2) receptor two-fold. In addition, the N439K mutation also confers resistance to neutralising antibodies being developed as treatments.
In a new paper published in Cell, an international team of researchers characterised how the N439K mutation affects SARS-CoV-2 infection. Despite other variants, including B.1.1.7 and B.1.351, garnering more attention, the N439K mutation is the second most common mutation in the receptor binding domain (RBD). It was first detected in Scotland in March 2020 and since then, a second lineage (B.1.258) has independently emerged in other European countries. By January 2021, the B.1.258 variant was detected in more than 30 countries across the globe.
But why is this variant important? According to the investigators, N439K mutants are similar to the wild-type virus in their virulence and ability to spread; however, they bind to the human ACE2 receptor with two-fold greater affinity and are somewhat resistant to many neutralising monoclonal antibodies, including one that is part of a treatment authorised for emergency use by the US Food and Drug Administration (FDA).
Gyorgy Snell, Senior Director of Structural Biology at Vir Biotechnology and the study’s senior author, explained that they unearthed “that the virus has many ways to alter the immunodominant domain to evade immunity while retaining the ability to infect and cause disease. A significant finding from this paper is the extent of variability found in the immunodominant receptor binding motif (RBM) on the Spike protein.”
The team used X-ray crystallography to determine how the altered structure of N439K RBM changes the interaction with ACE2. Snell commented: ” A single amino acid change (asparagine to lysine) enables the formation of a new point of contact with the ACE2 receptor, in line with the measured two-fold increase in binding affinity. Therefore, the mutation both improves interaction with the viral receptor ACE2 and evades antibody-mediated immunity.”
In the study the team also analysed the binding of >440 polyclonal sera samples and >140 monoclonal antibodies from recovered patients to the N439K variant. They found that a proportion of both monoclonal antibodies and serum samples were significantly less able to interact with viruses carrying the N439K mutation. In addition, and perhaps the most important finding, was that the N439K mutation allowed pseudoviruses to resist neutralisation by a monoclonal antibody that has been approved by the FDA for emergency use as part of a two-antibody cocktail. One way around this problem, said the researchers, could be the use of antibodies that target highly conserved sites on the RBM.
Snell concluded by saying that one of the greatest challenges when studying SARS-CoV-2 is the lack of sequencing that is currently being done: while more than 90 million cases of COVID-19 have been recorded, only about 350,000 virus variants have been sequenced. Snell remarked: “That is only 0.4 percent – just the tip of the iceberg. This underscores the need for broad surveillance, a detailed understanding of the molecular mechanisms of the mutations, and for the development of therapies with a high barrier to resistance against variants circulating today and those that will emerge in the future.”
Related topics
Analysis, Antibodies, Biologics, Cell-based assays, Disease Research, Drug Targets, Genomics, Immunology, In Vitro, Protein, Structural Biology, Therapeutics, X-ray Crystallography
Related conditions
Coronavirus, Covid-19
Related organisations
US Food and Drug Administration (FDA), Vir Biotechnology
Related people
Gyorgy Snell